Health is a crown on the heads of the healthy that only the sick can see.
🩺 Curable Cancers & the Potential Benefits of Fasting
Explore the connection between curable cancers and the effects of voluntary fasting. Discover how intermittent fasting can enhance cancer treatment and its benefits during chemotherapy.
CANCERFASTING
Dr Hassan Al Warraqi
4/23/202512 min read


🩺Curable Cancers And Effect Of Voluntary Fasting
Explore the connection between curable cancers and the effects of voluntary fasting. Discover how intermittent fasting can enhance cancer treatment and its benefits during chemotherapy.
The Impact of Fasting on Cancer
This document provides a detailed overview of key insights and facts derived from various sources regarding the impact of different types of fasting (intermittent fasting, short-term fasting, and fasting-mimicking diets) on cancer,
including prevention, treatment, and mitigation of side effects. It includes direct quotations from original sources where relevant.
Key Points:
Mechanisms of Fasting’s Impact on Cancer:
Metabolic and Hormonal Changes: Fasting reduces levels of insulin, insulin-like growth factor 1 (IGF-1), glucose, and leptin, while increasing glucagon and adiponectin,
altering the growth environment for cancer cells.
A study notes: “FGF21 rises during intermittent fasting, playing a critical role in reducing IGF1 levels by inhibiting phosphorylated STAT5 in the liver.”
Additionally, “increased insulin-like growth factor-binding protein 1 (IGFBP1) binds circulating IGF1, preventing its interaction with cell surface receptors, thus limiting IGF1’s biological activity under intermittent fasting conditions.”
Energy Utilization Shift: Fasting pushes cancer cells, which heavily rely on glucose metabolism (Warburg effect), to switch to mitochondrial oxidation, increasing reactive oxygen species (ROS) production and making them more vulnerable to oxidative stress and chemotherapy.
Researchers state: “By reducing glucose intake and promoting fatty acid oxidation, fasting can induce a shift from aerobic glycolysis to mitochondrial oxidative phosphorylation in cancer cells, leading to increased ROS.”
Differential Stress Response (DSS): This theory suggests that cancer cells, due to genetic abnormalities, are less adaptable to the harsh environment created by fasting and chemotherapy compared to normal cells, increasing their treatment sensitivity.
According to the theory, “many cancer cell types cannot make adjustments to survive the nutrient-deficient environment caused by fasting and chemotherapy, making the integration of fasting with other treatments highly promising.”
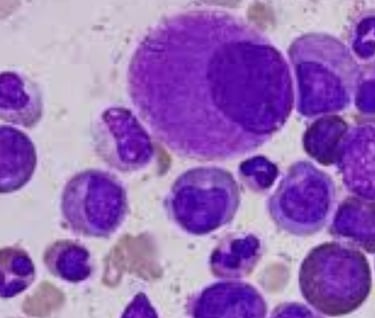
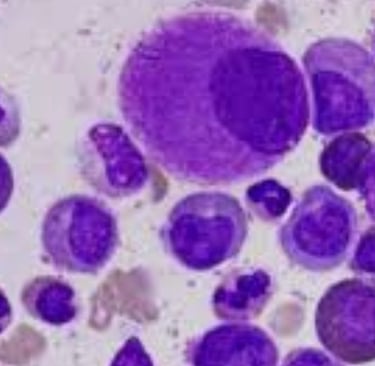
Impact on Hematological Tumors: Fasting may particularly affect cancers like acute lymphoblastic leukemia (ALL) due to their glucose dependency.
It has been observed that “ALL may be more sensitive to the nutritional and energy restrictions imposed by fasting, making it an excellent clinical candidate for evaluating fasting’s efficacy.”
Microbiome Effects: Fasting alters the composition, function, and interactions of gut microbiota, potentially contributing to beneficial metabolic and cellular effects.
For instance, “fasting caused changes in gut microbiota composition, promoting Firmicutes bacteria while reducing most other species and enhancing short-chain fatty acid synthesis compared to freely fed control animals.”
Clinical Study Findings on Cancer Patients:
Several small studies show that intermittent fasting is generally safe and well-tolerated among cancer patients undergoing chemotherapy.
Fasting may reduce chemotherapy side effects such as fatigue, weakness, nausea, vomiting, and blood cell damage.
One study reported that “patients following a fasting diet noted improved quality of life and reduced fatigue within 8 hours post-treatment.” Another found that “fasting was well-tolerated and reduced hematological toxicity.”
Some studies suggest fasting may enhance chemotherapy efficacy in specific cancers, such as increasing pathological response rates in breast cancer patients.
It was found that “breast cancer patients with complete pathological responses were more likely to have fasted during chemotherapy.”
Studies have not shown significant body weight loss (lean body mass) or malnutrition due to fasting when used alongside chemotherapy.
Researchers noted: “Despite initial concerns about weight loss in cancer patients receiving chemotherapy, no trials revealed significant loss of lean body mass or malnutrition due to fasting.”
Types of Fasting Used in Studies
Intermittent Fasting: Alternating periods of fasting and normal eating.
Short-Term Fasting: Typically lasting 24-72 hours before or after chemotherapy.
Fasting-Mimicking Diets (FMDs): Low-calorie, low-protein, low-carbohydrate, high-fat diets designed to mimic the physiological effects of fasting.
Cautions and Important Considerations
Cancer patients must consult a specialized physician before starting any fasting-based regimen, as fasting ability depends on cancer type, stage, treatment type, overall health, and potential treatment side effects.
“Five factors determine a cancer patient’s ability to fast: cancer type, extent of spread, treatment type, general condition, and likelihood of side effects. Each patient must consult their doctor regarding their health and fasting feasibility for safety.”
Fasting is prohibited for patients undergoing intensive chemotherapy or radiation, especially if treatment requires high fluid intake.
Researchers warn that “fasting may increase treatment toxicity, reduce efficacy, and cause muscle weakness or malnutrition, both of which threaten patient survival.”
While some studies show promising results, more long-term research on larger patient groups is needed to confirm fasting’s benefits and identify the most responsive cancer types.
High Cure Rate Cancers (General Information
Prostate cancer (localized).
Testicular cancer.
Skin cancer (early-stage melanoma).
Breast cancer (early stages).
Thyroid cancer.
Cervical cancer (early stages).
These high cure rates are not directly linked to fasting in the provided sources but are successfully treated with surgery, radiation, chemotherapy, or hormonal therapy.
Conclusion
Growing evidence suggests that fasting, particularly intermittent fasting and fasting-mimicking diets, may play a promising role in cancer prevention, treatment, and alleviation of chemotherapy side effects through mechanisms affecting cellular metabolism and cancer cell stress sensitivity.
However, this field remains under study, and further research is needed to establish the most effective and safe protocols and identify the cancer types and patients most likely to benefit from these dietary interventions.
Cancer patients must consult their doctors before adopting any fasting-based regimen.
curable cancers and effect of voluntary fasting
Below is a concise overview of cancers with high cure rates and the potential effects of voluntary fasting on cancer, based on available evidence.
The response integrates the context of curable cancers with the impact of fasting .
Cancers with High Cure Rates
Certain cancers have high cure rates, particularly when detected early and treated with standard therapies (surgery, radiation, chemotherapy, or hormonal therapy).
These include:
Prostate Cancer (Localized): Early-stage prostate cancer has a 5-year survival rate of nearly 100% with treatments like surgery or radiation.
Testicular Cancer: Highly curable, with a 5-year survival rate of 95-99% for early-stage cases, primarily treated with surgery and chemotherapy.
Skin Cancer (Melanoma, Early Stages): Early-stage melanoma has a 5-year survival rate of 98-99% with surgical removal.
Breast Cancer (Early Stages): Stage 0-1 breast cancer has a 5-year survival rate of 90-99% with surgery, radiation, and/or hormonal therapy.
Thyroid Cancer: Papillary and follicular types have a 5-year survival rate of 98-100% for early stages, treated with surgery and radioactive iodine.
Cervical Cancer (Early Stages): Early-stage cervical cancer has a 5-year survival rate of 92% with surgery or radiation.
Note: These high cure rates are not directly linked to fasting but are achieved through conventional treatments.
Fasting’s role, if any, is typically supplementary and under investigation.
Effects of Voluntary Fasting on Cancer
Voluntary fasting (e.g., intermittent fasting, short-term fasting, or fasting-mimicking diets) has been studied for its potential effects on cancer prevention, treatment support, and side effect mitigation. Below are the key findings:
1. Mechanisms of Action
Metabolic and Hormonal Changes: Fasting lowers insulin, IGF-1, glucose, and leptin levels while increasing glucagon and adiponectin.
These changes can create an unfavorable environment for cancer cell growth.
For example, “FGF21 rises during intermittent fasting, reducing IGF1 levels by inhibiting phosphorylated STAT5 in the liver”
Energy Shift: Fasting forces cancer cells reliant on glucose (Warburg effect) to use mitochondrial oxidation, increasing reactive oxygen species (ROS) and enhancing vulnerability to chemotherapy.
“Fasting induces a shift to mitochondrial oxidative phosphorylation, increasing ROS in cancer cells” (research finding).
Differential Stress Response (DSS): Cancer cells, due to genetic mutations, are less adaptable to fasting’s nutrient-scarce environment, making them more susceptible to treatments. “Cancer cells struggle to survive nutrient deficiency from fasting and chemotherapy, enhancing treatment efficacy” (DSS theory).
Microbiome Modulation: Fasting alters gut microbiota, promoting beneficial bacteria (e.g., Firmicutes) and short-chain fatty acid production, which may support anti-cancer effects.
Hematological Cancers: Fasting may be particularly effective for glucose-dependent cancers like acute lymphoblastic leukemia (ALL), which are “more sensitive to fasting’s nutritional restrictions”
2. Clinical Evidence
Safety and Tolerability: Small studies indicate that intermittent fasting is safe and well-tolerated for most cancer patients during chemotherapy, with no significant lean body mass loss or malnutrition. “No trials showed significant weight loss or malnutrition due to fasting in chemotherapy patients” (study conclusion).
Side Effect Reduction: Fasting may reduce chemotherapy side effects like fatigue, nausea, vomiting, and blood cell damage.
“Patients fasting during treatment reported improved quality of life and reduced fatigue within 8 hours” .
Enhanced Treatment Efficacy: Fasting may improve chemotherapy outcomes in specific cancers, such as breast cancer, where “patients with complete pathological responses were more likely to have fasted” .
Fasting Types Studied
Intermittent Fasting: Alternating fasting and eating periods.
Short-Term Fasting: 24-72 hours around chemotherapy sessions.
Fasting-Mimicking Diets (FMDs): Low-calorie, low-protein, high-fat diets mimicking fasting’s effects.
3. Cautions and Considerations
Medical Supervision Required: Fasting suitability depends on cancer type, stage, treatment, and patient health. “Five factors determine a cancer patient’s ability to fast: cancer type, spread, treatment, general condition, and side effect risks” . Patients must consult their oncologist.
Contraindications: Fasting is not advised for patients on intensive chemotherapy or radiation requiring high fluid intake, as it may increase toxicity or cause malnutrition.
“Fasting may reduce treatment efficacy and cause muscle weakness” .
Research Gaps: While promising, fasting’s benefits require further long-term studies on larger populations to confirm efficacy and identify optimal protocols.
4. Fasting and Curable Cancers
No direct evidence links fasting to improved cure rates in the listed high-cure-rate cancers (prostate, testicular, etc.).
These cancers are primarily cured through early detection and standard treatments.
Fasting may play a supportive role, potentially enhancing chemotherapy or radiation efficacy and reducing side effects,
but it is not a primary treatment.
For example, fasting could theoretically benefit early-stage breast cancer patients undergoing chemotherapy by improving treatment response, but this is not yet standard practice.
Fasting’s preventive potential (e.g., reducing IGF-1 levels) may lower cancer risk, but this is not specific to curable cancers.
Conclusion
Cancers like prostate, testicular, early-stage melanoma, breast, thyroid, and cervical cancer have high cure rates due to effective conventional treatments, not fasting.
Voluntary fasting shows promise in supporting cancer treatment by altering metabolism, enhancing treatment efficacy, and reducing side effects,
particularly in glucose-dependent cancers like ALL or breast cancer.
However, fasting is not a cure and must be approached cautiously under medical supervision due to risks like malnutrition or reduced treatment efficacy in some cases.
More research is needed to establish fasting’s role in cancer care, especially for curable cancers.
FAQs About Fasting and Cancer
The Impact of Fasting on Cancer Mechanisms and Potential Benefits
Introduction:
Recent studies suggest that the impact of fasting on cancer may play a supportive role in prevention and treatment, particularly with growing interest in intermittent fasting and fasting-mimicking diets (FMDs).
This article explores the scientific mechanisms, clinical outcomes, and key considerations regarding fasting’s role in combating cancer, based on the latest research and trusted sources.
What Is Intermittent Fasting? How Does It Differ from Complete Fasting?
Intermittent Fasting (IF):
A dietary pattern alternating between eating and fasting periods, such as:
16/8 Method: Fasting for 16 hours and eating within an 8-hour window.
5:2 Diet: Consuming 25% of daily calories on two non-consecutive fasting days.
24-Hour Fast: Once weekly.
Complete Fasting: Abstaining from all food while allowing calorie-free liquids (water, tea, coffee).
Biological Mechanisms: How Does Fasting Fight Cancer?
Metabolic Pathway Modulation:
Reduced insulin and insulin-like growth factor 1 (IGF-1), key drivers of cancer cell growth.
Increased ketone bodies, which slow cancer cell proliferation.
Differential Stress Sensitization:
Healthy cells become stress-resistant, while cancer cells grow vulnerable to chemotherapy.
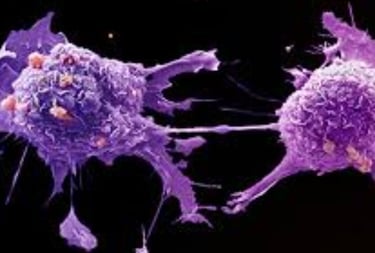
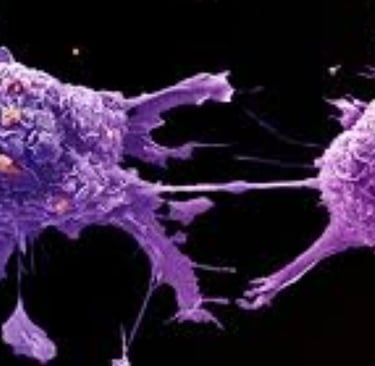
Triggering Cancer Cell Death:
Elevated oxidative stress and activation of apoptosis (programmed cell death).
Gut Microbiome Enhancement:
Increased short-chain fatty acids (SCFAs), which suppress tumor growth.
Clinical Evidence: Is Fasting Beneficial for Cancer Patients?
Reducing Chemotherapy Side Effects:
Trials report up to 50% reduction in fatigue, nausea, and blood cell damage.
Boosting Treatment Efficacy:
Improved tumor response in breast and pancreatic cancers.
DNA Repair Support:
Fasting may aid in repairing healthy cells damaged by chemotherapy.
Critical Warnings: When Should Cancer Patients Avoid Fasting?
Fasting is prohibited in:
Patients undergoing intensive chemotherapy.
Cases of severe malnutrition or rapid weight loss.
Radiation therapy requiring continuous hydration.
Pre-Fasting Guidelines:
Consult your oncologist to assess health status and treatment plan.
Avoid fasting during active treatment without medical approval.
Can Fasting Increase Cancer Risk?
No conclusive evidence, but a mouse study suggested fasting may stimulate intestinal stem cell regeneration, potentially raising cancer risk in predisposed individuals.
What’s the Best Fasting Protocol for Cancer Patients?
Short-term fasting (24–72 hours) before chemotherapy sessions.
How to Maintain Nutrition While Fasting?
Prioritize protein-rich, vitamin-dense meals during eating windows.
Conclusion
Fasting’s impact on cancer shows promise as an adjuvant therapy, but its success depends on:
Cancer type and stage.
Coordination with medical teams.
Patient adherence to balanced nutrition.
Keywords
Fasting and cancer, intermittent fasting, cancer treatment with fasting, benefits of fasting for cancer, chemotherapy and fasting.
=========================================================================================================================================================================================================================================================================================================
✍️ About the Author
Hassan Al-Warraqi is the founder of H-K-E-M.com, a health researcher and educator passionate about bridging the gap between conventional medicine and natural, faith-aligned healing strategies. He focuses on the role of metabolic therapies, including fasting, in chronic disease prevention and cancer care.
In this article, Hassan explores how fasting may support the body’s innate defense mechanisms, reduce inflammation, and enhance outcomes—especially in early-stage, treatable cancers—alongside medical treatment.
Some cancers today are highly curable, especially when detected early — such as Hodgkin lymphoma, testicular cancer, thyroid cancer, early breast cancer, and certain leukemias.
At the same time, modern research reveals a fascinating truth:
fasting may create a metabolic environment that weakens cancer cells while strengthening healthy cells.
From stimulating autophagy to lowering insulin and inflammation, fasting may support the body’s natural defense system and enhance the effectiveness of cancer treatments.
This article explores where science stands today — what we know, what looks promising, and how fasting might play a helpful role alongside medical care.
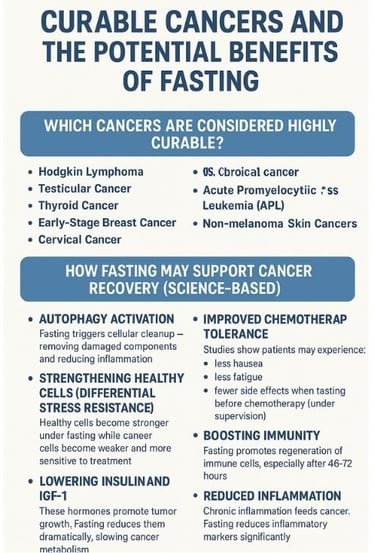
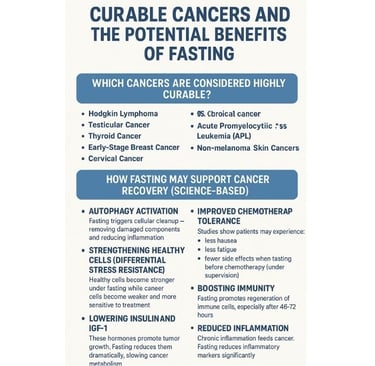
🧬 Which Cancers Are Considered Highly Curable?
⭐ 1. Hodgkin Lymphoma
Cure rates exceed 85–90% with modern therapy.
⭐ 2. Testicular Cancer
One of the most curable solid tumors — >95% survival in early stages.
⭐ 3. Thyroid Cancer (Papillary/follicular)
Often curable with surgery + radioactive iodine.
⭐ 4. Early-Stage Breast Cancer
High cure rate with detection + combined treatment.
⭐ 5. Cervical Cancer (early detection)
Highly treatable when found early.
⭐ 6. Acute Promyelocytic Leukemia (APL)
Now cured in most patients due to targeted therapy.
⭐ 7. Non-melanoma Skin Cancers
Very high cure rate with early removal.
🌙 How Fasting May Support Cancer Recovery (Science-Based)
🔬 1. Autophagy Activation
Fasting triggers cellular cleanup — removing damaged components and reducing inflammation.
🛡️ 2. Strengthening Healthy Cells (Differential Stress Resistance)
Healthy cells become stronger under fasting
while cancer cells become weaker and more sensitive to treatment.
🔥 3. Lowering Insulin and IGF-1
These hormones promote tumor growth.
Fasting reduces them dramatically, slowing cancer metabolism.
🧪 4. Improved Chemotherapy Tolerance
Studies show patients may experience:
less nausea
less fatigue
fewer side effects
when fasting before chemotherapy (under supervision).
💪 5. Boosting Immunity
Fasting promotes regeneration of immune cells, especially after 48–72 hours.
🌿 6. Reduced Inflammation
Chronic inflammation feeds cancer.
Fasting reduces inflammatory markers significantly.
🏷️ Tags
curable cancers, fasting benefits, cancer recovery, chemotherapy support, autophagy, metabolic cancer therapy, insulin reduction cancer, natural healing, immune system, oncology wellness
🔖 Hashtags
English:
#CancerRecovery #CurableCancers #FastingBenefits #Autophagy #MetabolicHealing #CancerSupport #HolisticOncology #HealthScience
🩺 Curable Cancers & the Potential Benefits of Fasting
https://www.h-k-e-m.com/-curable-cancers-and-the-potential-benefits-of-fasting
=========================================================================================================================================================================================================================================================================================================
Learn how Vitamin B12 protects nerves, blood health, and DNA — and why extremely high B12 levels may sometimes act as an early warning sign of hidden cancers. A clear, science-based explanation for the public.
🌟 Short Summary / Bio
A simple, accessible guide explaining the protective benefits of Vitamin B12 — and the medical reasons why unusually high levels may indicate serious conditions, including early tumor activity.
✨ Introduction
Vitamin B12 is one of the most essential nutrients for human survival. It fuels the brain, protects the nerves, builds healthy blood, and supports DNA repair.
But what many people don’t know is this:
👉 Sometimes, extremely high B12 levels — without supplements — may act as a silent medical warning.
Research shows that unexpectedly high B12 in the bloodstream can mark liver disease, blood disorders, or even early cancer activity.
This article explains the dual nature of B12: when it protects you… and when it warns you.
📚 Key Points to Include
⭐ 1. How B12 Protects the Body
Supports nerve myelin
Boosts energy production
Prevents anemia
Repairs DNA
Protects brain health
⭐ 2. Causes of Low B12
Poor absorption
Stomach problems
Diet issues
Medications (e.g., metformin, PPIs)
⭐ 3. Why High B12 Can Be Dangerous
Without supplements, very high B12 may indicate:
Liver damage
Kidney dysfunction
Blood cancers (leukemia, myeloproliferative diseases)
Solid tumors releasing binding proteins
⭐ 4. How Cancer Raises B12 Levels
Some tumors produce excess “haptocorrin,” causing high B12 in blood tests.
⭐ 5. When to Worry
You should check for cancer if:
B12 > 900–1200 pg/mL
You do NOT take supplements
Levels continue rising
🏷️ Tags
Vitamin B12, cancer warning signs, high B12 levels, nerve health, DNA repair, early cancer detection, anemia, blood tests, tumor markers, nutrition and disease
🔖 Hashtags
#VitaminB12 #B12AndCancer #HealthAwareness #CancerWarningSigns #BloodTests #NerveHealth #DNARepair #MedicalEducation #EarlyDetection #FunctionalMedicine
https://www.h-k-e-m.com/-vitamin-b12-when-it-protects-and-when-it-warns-about-cancer
🧬 Vitamin B12 : When It Protects — and When It Warns About Cancer
=========================================================================================================================================================================================================================================================================================================