what is the post-stroke-stroke : fasting
Learn about the different types of stroke, prevention strategies, treatment options, and post-stroke management including taking medications, exercising, eating a healthy diet, and managing stress....
NERVOUS SYSTEM
Dr Hassan Al Warraqi


Understanding Stroke : Post-stroke-stroke
Post-stroke-stroke Types, Prevention, and Treatment
A stroke & post-stroke stroke
is a medical emergency that occurs when the blood supply to part of the brain is interrupted or reduced,
Depriving brain tissue of oxygen and nutrients.
Within minutes, brain cells begin to die.
A stroke can cause lasting brain damage, disability, or even death.
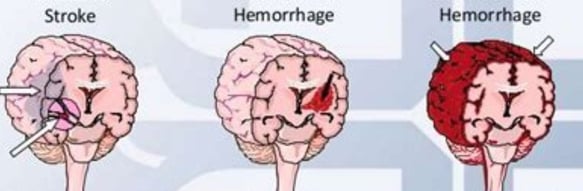
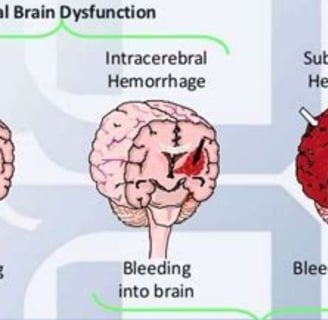
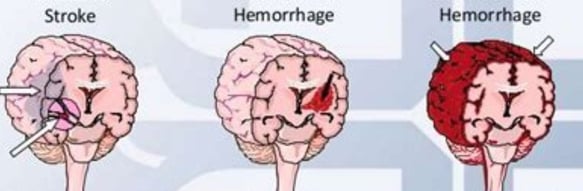
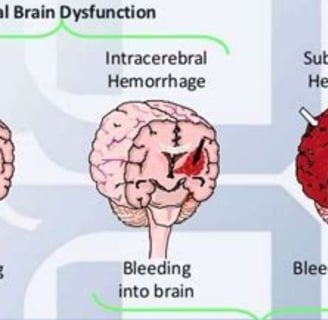
There are two main types of stroke:
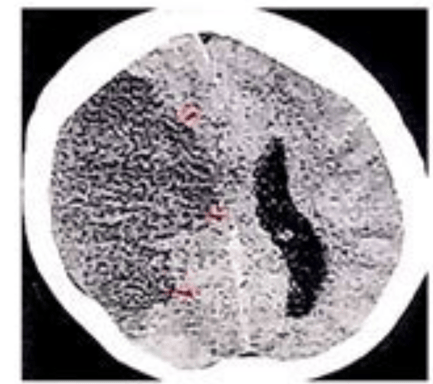
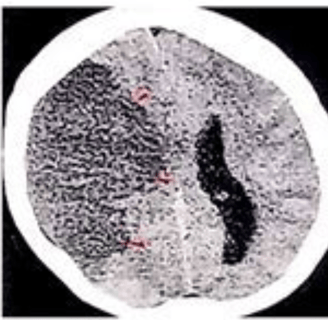
Ischemic stroke: This is the most common type of stroke, accounting for about 87% of all strokes. It occurs when a blood clot blocks a blood vessel leading to the brain.
Hemorrhagic stroke: This type of stroke occurs when a blood vessel in the brain ruptures and bleeds into the surrounding brain tissue.
Strokes can happen to anyone, at any age. However, the risk of stroke increases with age.
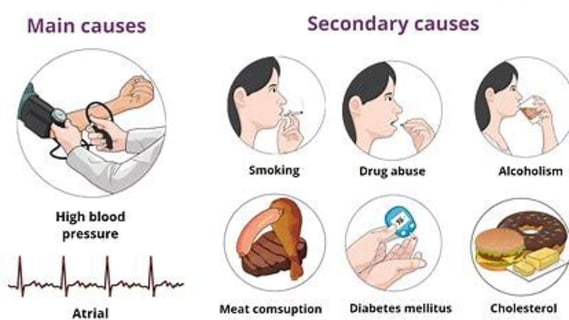
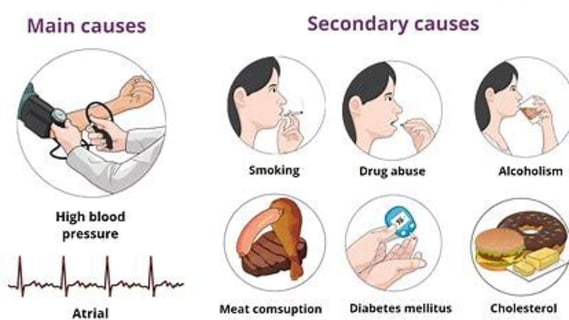
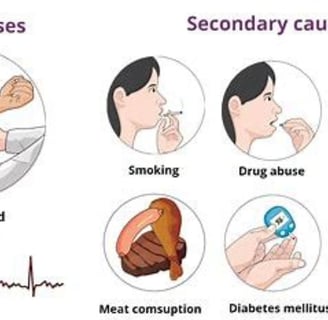
Other risk factors for stroke include:
High blood pressure
High cholesterol
Heart disease
Diabetes
Smoking
Obesity
Physical inactivity
Family history of stroke
high stress condition
vascular problem
addiction captogin
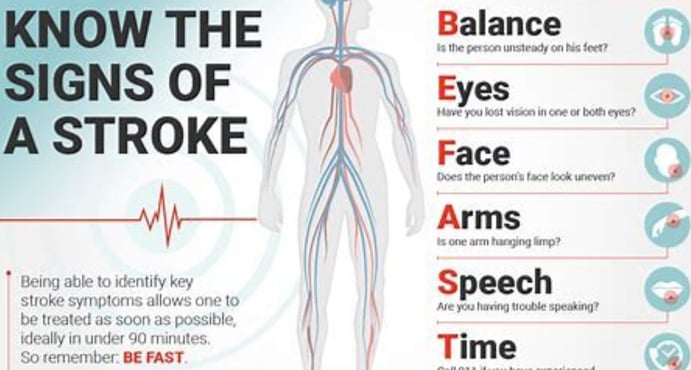
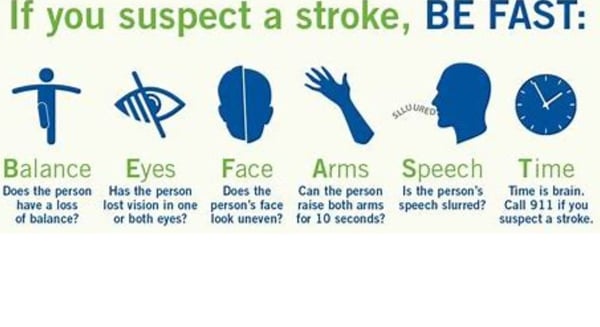
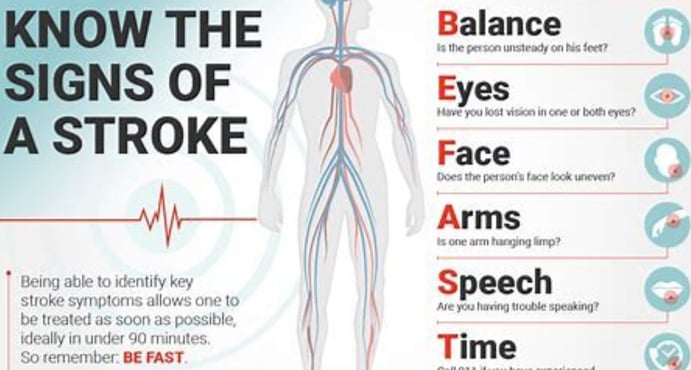
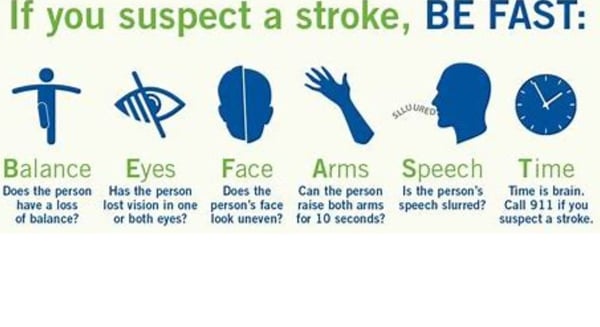
Symptoms of stroke
The symptoms of stroke can vary depending on the part of the brain that is affected. However, common symptoms include:
Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body
Sudden confusion, trouble speaking or understanding speech
Sudden trouble seeing in one or both eyes
Sudden trouble walking, dizziness, loss of balance or coordination
Sudden severe headache with no known cause
increased blood sugar
trouble sleeping
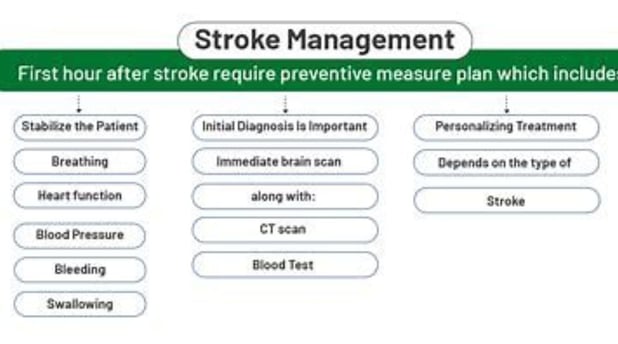
Treatment for stroke
The treatment for stroke depends on the type of stroke and the severity of the symptoms.
For ischemic stroke, the goal of treatment is to dissolve the blood clot and restore blood flow to the brain as quickly as possible. This can be done with medication or surgery.
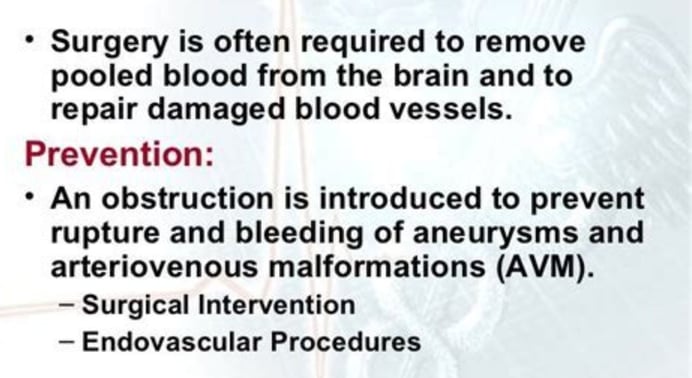
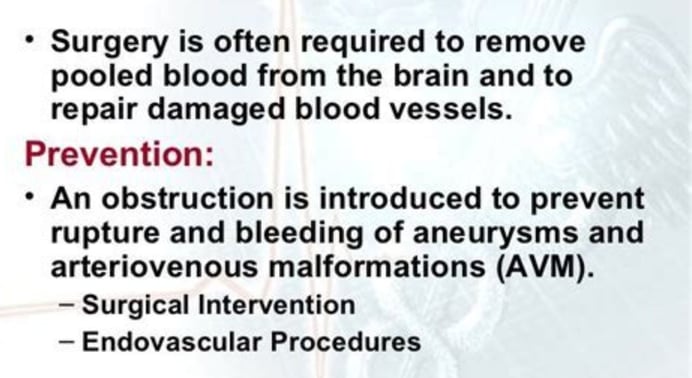
For hemorrhagic stroke, the goal of treatment is to stop the bleeding and reduce pressure on the brain. This may involve medication, surgery, or both.
Prevention of stroke
The best way to prevent stroke is to control your risk factors. This includes:
Maintaining a healthy blood pressure
Keeping your cholesterol levels under control
Managing diabetes
Quitting smoking
Maintaining a healthy weight
Exercising regularly
Eating a healthy diet
Quitting alcohol
Quitting uneasily medicine like antihistamines
Post-stroke treatment
is focused on helping you recover as much function as possible and return to independent living.
The impact of the stroke depends on the area of the brain involved and the amount of tissue damaged. Some people may make a full recovery, while others may have permanent disabilities.
Post-stroke treatment typically begins in the hospital and continues at home or in a rehabilitation facility.
Some common post-stroke treatments include:
Physical therapy: Physical therapy can help you improve your mobility, balance, and coordination.
Occupational therapy: Occupational therapy can help you learn to perform everyday activities again, such as bathing, dressing, and eating.
Speech therapy: Speech therapy can help you improve your communication skills, including speaking, writing, and understanding speech.
Cognitive rehabilitation: Cognitive rehabilitation can help you improve your memory, thinking skills, and problem-solving abilities.
Medications: Medications may be used to control risk factors for stroke, such as high blood pressure, high cholesterol, and diabetes.
Medications may also be used to treat specific complications of stroke, such as depression and seizures.
In addition to medical treatment, there are a number of things you can do at home to help your recovery, such as:
Eating a healthy diet: Eating a healthy diet can help you maintain a healthy weight, control your blood pressure and cholesterol levels, and reduce your risk of complications from stroke.
Exercising regularly: Exercise can help you improve your cardiovascular health, strength, and flexibility.
Getting enough sleep: Sleep is essential for healing and recovery.
Managing stress: Stress can worsen the effects of stroke. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Staying connected with friends and family: Social support can help you stay motivated and positive during your recovery.
Post-stroke stroke
also known as recurrent stroke or secondary stroke, is a stroke that occurs after a previous stroke. It is estimated that 10-20% of people who have a stroke will have a recurrent stroke within 5 years.
There are a number of factors that can increase the risk of post-stroke stroke, including:
Age: The risk of post-stroke stroke increases with age.
Severity of the initial stroke: People who have had a more severe stroke are at higher risk of having a recurrent stroke.
Presence of risk factors for stroke: People who have risk factors for stroke, such as high blood pressure, high cholesterol, and diabetes, are at higher risk of having a recurrent stroke.
Lack of adherence to post-stroke treatment: People who do not adhere to their post-stroke treatment, such as taking medications, exercising, and eating a healthy diet, are at higher risk of having a recurrent stroke.
stress more stress more stroke .
The symptoms of post-stroke stroke are the same as the symptoms of any stroke.
If you have had a stroke, it is important to work with your doctor to reduce your risk of having a recurrent stroke.
This may involve taking medications, exercising, eating a healthy diet, and managing stress.Other measures.
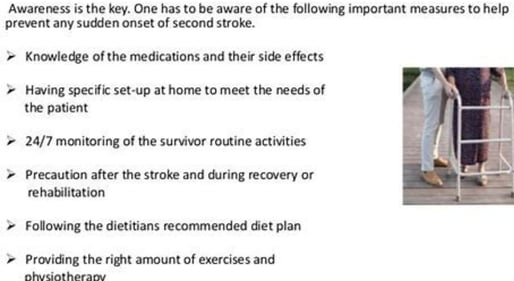
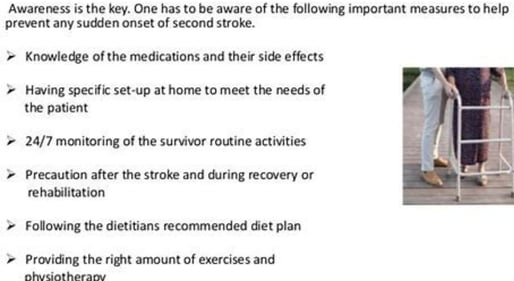
Here are some tips for preventing post-stroke stroke:
Take all of your medications as prescribed by your doctor.
Exercise regularly. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Eat a healthy diet that is low in saturated and trans fats and high in fruits, vegetables, and whole grains.
Manage stress. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Get regular medical checkups. See your doctor regularly to monitor your health and manage your risk factors for stroke.
Islamic fasting is the general treatment of great and guaranteed benefit.
fasting
There is growing interest in the potential health benefits of fasting, including for people who have had a stroke.
Some studies have shown that fasting can help to improve brain function,
reduce inflammation, and
protect against neurodegenerative diseases.
One study found that intermittent fasting (IF) improved cognitive function and reduced the risk of stroke in mice.
Another study found that IF protected against brain damage in rats that had a stroke.
Here are some things to keep in mind if you are considering fasting after a stroke:
Fasting can lead to dehydration, which can be dangerous for people who have had a stroke. It is important to drink plenty of fluids while fasting.
Fasting can also lower blood sugar levels, which can be dangerous for people who have diabetes or are taking insulin.
It is important to monitor your blood sugar levels closely while fasting.
Fasting can also interact with medications, so it is important to talk to your doctor before starting any fasting regimen.
If you decide to fast after a stroke, it is important to start slowly and gradually increase the length of your fasts.
It is also important to listen to your body and break your fast if you feel unwell.
Here are some tips for fasting safely:
Start with a short fast, such as 12 hours. Gradually increase the length of your fasts as you become more comfortable.
Listen to your body. If you feel lightheaded, dizzy, or unwell, break your fast.
Stay hydrated. Drink plenty of fluids while fasting. Water is best, but you can also drink unsweetened tea or coffee.
Eat a healthy diet when you break your fast. When you break your fast, it is important to eat a healthy meal that is high in protein and fiber.
fasting islamic in strokes
Fasting is a practice of abstaining from food and drink for a period of time.
It is a common practice in many religions, including Islam.
In Islam, fasting is a pillar of faith and is observed during the month of Ramadan. During Ramadan, Muslims fast from dawn to dusk.
There is some evidence to suggest that fasting may be beneficial for people who have had a stroke.
One study found that fasting improved cognitive function and reduced the risk of stroke in mice. Another study found that fasting protected against brain damage in rats that had a stroke.
Islamic fasting is the general treatment of great and guaranteed benefit.
However, more research is needed to confirm the long-term safety and efficacy of fasting for people who have had a stroke.
Here are some things to keep in mind if you are considering fasting after a stroke:
Fasting can lead to dehydration, which can be dangerous for people who have had a stroke. It is important to drink plenty of fluids while fasting.
Fasting can also lower blood sugar levels, which can be dangerous for people who have diabetes or are taking insulin. It is important to monitor your blood sugar levels closely while fasting.
Fasting can also interact with medications, so it is important to talk to your doctor before starting any fasting regimen.
If you decide to fast after a stroke, it is important to start slowly and gradually increase the length of your fasts. It is also important to listen to your body and break your fast if you feel unwell.
Here are some tips for fasting safely:
Start with a short fast, such as 12 hours. Gradually increase the length of your fasts as you become more comfortable.
Listen to your body. If you feel lightheaded, dizzy, or unwell, break your fast.
Stay hydrated. Drink plenty of fluids while fasting. Water is best, but you can also drink unsweetened tea or coffee.
Eat a healthy diet when you break your fast. When you break your fast, it is important to eat a healthy meal that is high in protein and fiber.
keywords
stroke, brain attack, Ischemic ,Hemorrhagic, fasting . if .post-stroke stroke, prevention . treatment ,taking medications, exercising, eating a healthy diet, and managing stress.Other measures,
Deep Dive: Stroke, Its Management, and Beyond
This document provides a comprehensive overview of key insights and facts about stroke, drawn from various sources, covering post-stroke quality of life assessment, rehabilitation, modern treatments, nutrition, complications, recovery stories, and patients’ rights and available services.
1. Quality of Life Assessment for Post-Stroke Patients with Vertigo:
that most post-stroke patients with vertigo have a moderate quality of life, with a small percentage experiencing poor quality.
The study recommended identifying and modifying factors affecting quality of life to improve early diagnosis and support patients through rehabilitation programs.
It emphasized developing effective compensatory strategies to restore sensory integration and balance.
The World Health Organization defines quality of life as individuals’ perception of their position in life within the context of their culture, values, goals, and expectations.
Vertigo, a common post-stroke symptom, is closely linked to balance loss and increased fall risk, negatively impacting quality of life.
The study highlighted the theoretical importance of addressing post-stroke effects on bodily functions, particularly balance disorders and vertigo, which complicate daily activities.
Methodology: The study included 40 post-stroke vertigo patients at Tishreen University Hospital, using a questionnaire (European Quality of Life 5 Dimensions - EQ-5D) to assess general quality of life and collect demographic data.
Results: Significant differences in quality of life were observed based on age and family size, with better outcomes in the 46-57 age group and those with smaller families (3-5 members).
Chronic disabilities, especially in routine activities, were shown to impact quality of life, with balance and motor coordination issues limiting independence.
The study concluded the need for early intervention, appropriate care, and tailored educational and rehabilitation programs for stroke patients.
2. Post-Stroke Rehabilitation:
Rehabilitation aims to help patients regain lost skills, improve movement, speech, strength, daily living abilities, independence, and quality of life.
Research shows better outcomes for those in intensive rehabilitation programs.
Rehabilitation involves targeted, repetitive activities based on the affected body part or ability.
It includes physical activities like motor skill exercises, constraint-induced therapy, and range-of-motion treatments.
Technological aids such as functional electrical stimulation, robotics, wireless technology, and virtual reality may be used.
Cognitive and psychological activities address cognitive impairments, communication, psychological evaluation, and medication.
Rehabilitation typically begins within 24-48 hours of a stroke during hospitalization and may continue for months or years depending on stroke severity and complications.
It occurs in various settings, including inpatient/outpatient rehabilitation units, skilled nursing facilities, and home-based programs.
A multidisciplinary team, including physicians, rehabilitation nurses, physical and occupational therapists, speech-language pathologists, social workers, psychologists, and vocational counselors, is involved.
Outcomes depend on physical, emotional, social, and therapeutic factors.
3. Modern Advances in Stroke Treatment:
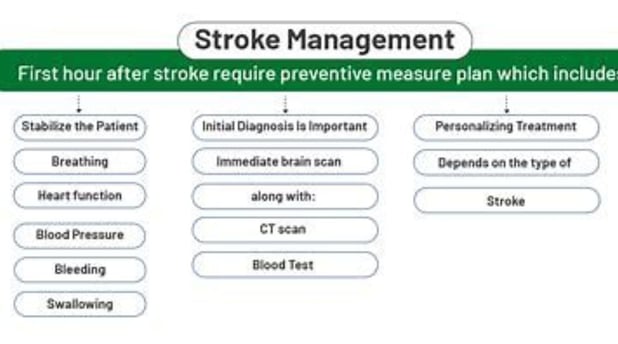
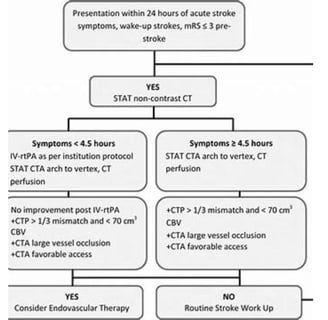
Rapid, accurate diagnosis is the critical first step in stroke management.
Diagnostic services include brain Doppler ultrasound, cerebral angiography, and nerve/muscle testing.
Recent advances include:
Stem Cell Therapy: Aims to regenerate damaged brain tissue, showing improvements in motor and cognitive functions and reduced psychological symptoms.
Repetitive Transcranial Magnetic Stimulation (rTMS): A non-invasive technique using magnetic fields to stimulate brain areas, aiding motor and cognitive recovery and alleviating depression.
Mechanical Thrombectomy: An effective intervention for ischemic stroke, removing blood clots blocking cerebral arteries.
Advanced Medications: Anticoagulants (e.g., Apixaban) and clot-dissolving drugs (e.g., Tenecteplase) improve recovery and reduce long-term complications.
Modern rehabilitation techniques include functional electrical stimulation, robotic-assisted therapy, virtual reality, and transcranial magnetic stimulation.
A comprehensive approach combining rapid diagnosis, innovative treatments, and effective rehabilitation can transform stroke care outcomes.
4. Nutrition After Stroke:
A healthy diet and regular exercise are vital for recovery.
Patients with swallowing difficulties may require softer foods and thicker liquids.
General healthy eating recommendations include consuming whole grains, fruits, vegetables, adequate water, and a diet low in saturated fats, sugar, and salt.
Daily exercise is crucial, with home exercise programs advised by the rehabilitation team.
Maintaining a healthy weight is important, with BMI monitoring by a physician.
Avoid high-sodium foods to reduce sodium intake.
Reading food labels helps make healthier choices.
Dietary group recommendations outline preferred and limited/avoided options for dairy, protein, fruits, vegetables, grains, and more.
5. Stroke Complications:
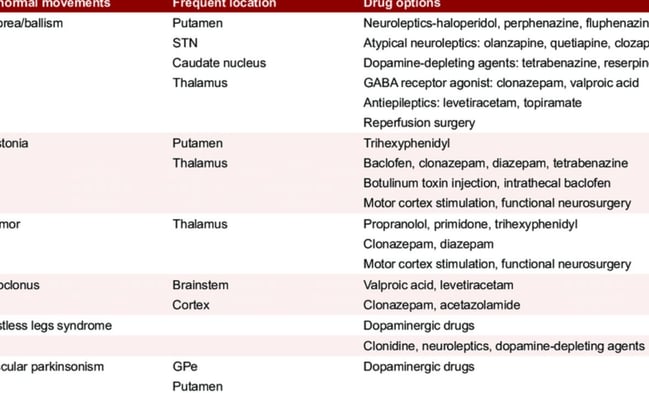
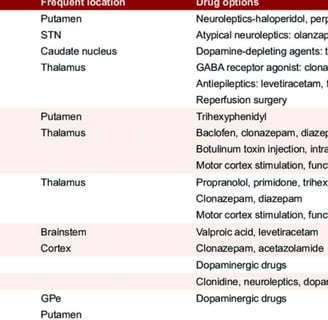
Stroke leads to complications affecting patients’ lives, including speech/expression difficulties, swallowing issues, memory problems, muscle weakness/spasticity, venous thrombosis, depression/mood swings, chronic headaches, lung/urinary infections, heart clots/arrhythmias, internal bleeding, urinary incontinence, falls/fractures, and seizures.
Prevention involves a balanced diet, regular exercise, avoiding smoking/alcohol, and managing risk factors like hypertension.
6. Psychological Support for Patients:
Long-term physical therapy can lead to loss of hope, making psychological and emotional support essential.
Key support providers include family, treating physicians, physical therapists, and psychologists.
Family: Provides a calm environment, monitors psychological changes, assists with daily tasks, acknowledges progress, and promotes social integration.
Physician: Highlights positive developments and reassures patients about overcoming challenges.
Physical Therapist: Maintains communication, offers support, and encourages patients.
Psychologist: Diagnoses conditions, determines optimal treatments, addresses psychological/social issues, suggests alternatives, and manages treatment side effects.
7. Post-Stroke Management:
Relies on integrated strategies to enhance quality of life and prevent complications.
Includes physical therapy to restore movement, strength, and flexibility; occupational therapy for daily activities; speech therapy for communication and swallowing; medication management to prevent recurrence and control risk factors; psychological/social support via counseling and support groups; long-term rehabilitation; and lifestyle changes like healthy eating, exercise, and quitting smoking.
Requires ongoing follow-up with specialists.
8. Stroke Recovery Stories:
Inspiring stories, like those of Ahmed Al-Amari, Fatima Ahmed, and Sami Jad, highlight the importance of rapid medical intervention, intensive rehabilitation, and family support.
Effective treatments included physical therapy, speech exercises, electrical stimulation, and comprehensive rehabilitation.
Prevention tips: maintain a healthy lifestyle (diet, exercise, no smoking) and regular medical check-ups to detect risk factors early.
9. Rights and Services for Stroke Patients
Patients requiring lifelong medications may receive higher payment caps for drugs.
Disability benefit recipients are exempt from certain healthcare fund service fees.
Recognized rehabilitation patients are entitled to inpatient/community rehabilitation, physical therapy, and home treatment units.
Those affected post-retirement may receive nursing and mobility benefits.
Work-related strokes qualify for occupational injury benefits.
Patients with a medical disability of 89% or higher may receive income tax exemptions.
Discounts on purchase taxes, approval fees, and municipal taxes (Arnona) are available for recognized disabled individuals.
Those with mobility limitations may receive housing adaptation assistance, vocational rehabilitation, and community support services.
Conclusion:
Managing stroke requires a holistic approach encompassing accurate medical assessment, timely acute-phase treatment, intensive and ongoing rehabilitation, psychological and social support, proper nutrition, lifestyle adjustments, and awareness of patients’ rights and services.
Advances in treatment, diagnosis, and rehabilitation offer hope for improved outcomes, reduced disability, and enhanced quality of life for patients and their families.
Deep Dive: Frequently Asked Questions About Stroke and Its Management
What is a stroke, and what are its main types?
A stroke occurs when blood flow to the brain is disrupted, causing nerve cell damage. The two main types are:
Ischemic Stroke: The most common, caused by a blockage in blood vessels preventing blood from reaching part of the brain.
Hemorrhagic Stroke: Results from a ruptured blood vessel in the brain, leading to bleeding.
What symptoms require immediate medical attention when a stroke is suspected?
Key symptoms include facial drooping, arm weakness, and speech difficulties. Even if these symptoms are temporary (as in a transient ischemic attack), immediate emergency contact is critical, as the risk of a full stroke increases in the days or weeks following.
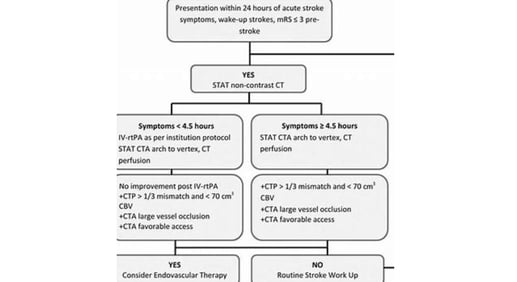
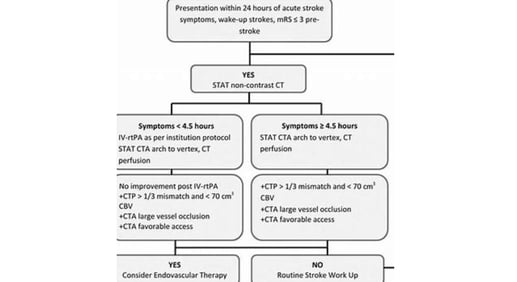
What are the immediate treatment options for ischemic stroke?
The goal of urgent treatment is to restore blood flow to the brain quickly. Options include:
Intravenous Medications: Clot-dissolving drugs like tissue plasminogen activator, administered within 4.5 hours of symptom onset.
Endovascular Interventions: Delivering medications directly to the brain or mechanically removing the clot using a catheter.
What is the role of rehabilitation after a stroke, and what does it involve?
Post-stroke rehabilitation is a comprehensive program to help patients regain lost skills and improve quality of life. It includes:
Physical Therapy: To restore movement, balance, and strength.
Occupational Therapy: To recover the ability to perform daily activities.
Speech and Language Therapy: To enhance communication and swallowing.
Psychological and Social Support: To help patients adapt to changes.
Rehabilitation typically begins in the hospital once the patient stabilizes and may continue for months or years.
How do diet and exercise impact recovery and prevention after a stroke?
Diet: A balanced diet low in saturated fats and sodium, and rich in fiber, fruits, and vegetables, helps control risk factors like high blood pressure and cholesterol. Patients with swallowing difficulties may need modified food textures or liquids under specialist supervision.
Exercise: Regular physical activity aids in regaining strength, flexibility, and balance, and reduces the risk of recurrent strokes. Daily tailored exercise programs are essential.
What are some potential complications of a stroke, and how are they managed?
Complications may include speech/swallowing difficulties, memory issues, muscle weakness/spasticity, depression, and increased risks of venous thrombosis or infections. Management requires a multidisciplinary team providing:
Targeted exercises.
Medications to control symptoms.
Compensatory strategies to improve function.
What are the latest advancements in stroke treatment?
Recent advancements include:
Stem Cell Therapy: To regenerate damaged brain tissue.
Repetitive Transcranial Magnetic Stimulation (rTMS): To enhance motor and cognitive functions.
Mechanical Thrombectomy: For precise clot removal.
Advanced Medications: More effective anticoagulants and clot-dissolving drugs.
Diagnostic Services: Brain Doppler ultrasound and cerebral angiography for rapid, accurate diagnosis.
What is the critical role of psychological and social support in stroke recovery?
Psychological and social support is vital for overcoming emotional challenges like depression, anxiety, and feelings of helplessness. It involves:
Support from family and friends to boost confidence and social integration.
Contributions from psychologists and support groups to improve emotional well-being.
Encouraging patients to achieve small goals and celebrating progress, which enhances rehabilitation commitment and overall quality of life.













Understanding Stroke : Post-stroke-stroke
Post-stroke-stroke Types, Prevention, and Treatment
A stroke & post-stroke stroke
is a medical emergency that occurs when the blood supply to part of the brain is interrupted or reduced,
Depriving brain tissue of oxygen and nutrients.
Within minutes, brain cells begin to die.
A stroke can cause lasting brain damage, disability, or even death.
There are two main types of stroke:
Ischemic stroke: This is the most common type of stroke, accounting for about 87% of all strokes. It occurs when a blood clot blocks a blood vessel leading to the brain.
Hemorrhagic stroke: This type of stroke occurs when a blood vessel in the brain ruptures and bleeds into the surrounding brain tissue.
Strokes can happen to anyone, at any age. However, the risk of stroke increases with age.
Other risk factors for stroke include:
High blood pressure
High cholesterol
Heart disease
Diabetes
Smoking
Obesity
Physical inactivity
Family history of stroke
high stress condition
vascular problem
addiction captogin
Symptoms of stroke
The symptoms of stroke can vary depending on the part of the brain that is affected. However, common symptoms include:
Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body
Sudden confusion, trouble speaking or understanding speech
Sudden trouble seeing in one or both eyes
Sudden trouble walking, dizziness, loss of balance or coordination
Sudden severe headache with no known cause
increased blood sugar
trouble sleeping
Treatment for stroke
The treatment for stroke depends on the type of stroke and the severity of the symptoms.
For ischemic stroke, the goal of treatment is to dissolve the blood clot and restore blood flow to the brain as quickly as possible. This can be done with medication or surgery.
For hemorrhagic stroke, the goal of treatment is to stop the bleeding and reduce pressure on the brain. This may involve medication, surgery, or both.
Prevention of stroke
The best way to prevent stroke is to control your risk factors. This includes:
Maintaining a healthy blood pressure
Keeping your cholesterol levels under control
Managing diabetes
Quitting smoking
Maintaining a healthy weight
Exercising regularly
Eating a healthy diet
Quitting alcohol
Quitting uneasily medicine like antihistamines
Post-stroke treatment
is focused on helping you recover as much function as possible and return to independent living.
The impact of the stroke depends on the area of the brain involved and the amount of tissue damaged. Some people may make a full recovery, while others may have permanent disabilities.
Post-stroke treatment typically begins in the hospital and continues at home or in a rehabilitation facility.
Some common post-stroke treatments include:
Physical therapy: Physical therapy can help you improve your mobility, balance, and coordination.
Occupational therapy: Occupational therapy can help you learn to perform everyday activities again, such as bathing, dressing, and eating.
Speech therapy: Speech therapy can help you improve your communication skills, including speaking, writing, and understanding speech.
Cognitive rehabilitation: Cognitive rehabilitation can help you improve your memory, thinking skills, and problem-solving abilities.
Medications: Medications may be used to control risk factors for stroke, such as high blood pressure, high cholesterol, and diabetes.
Medications may also be used to treat specific complications of stroke, such as depression and seizures.
In addition to medical treatment, there are a number of things you can do at home to help your recovery, such as:
Eating a healthy diet: Eating a healthy diet can help you maintain a healthy weight, control your blood pressure and cholesterol levels, and reduce your risk of complications from stroke.
Exercising regularly: Exercise can help you improve your cardiovascular health, strength, and flexibility.
Getting enough sleep: Sleep is essential for healing and recovery.
Managing stress: Stress can worsen the effects of stroke. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Staying connected with friends and family: Social support can help you stay motivated and positive during your recovery.
Post-stroke stroke
also known as recurrent stroke or secondary stroke, is a stroke that occurs after a previous stroke. It is estimated that 10-20% of people who have a stroke will have a recurrent stroke within 5 years.
There are a number of factors that can increase the risk of post-stroke stroke, including:
Age: The risk of post-stroke stroke increases with age.
Severity of the initial stroke: People who have had a more severe stroke are at higher risk of having a recurrent stroke.
Presence of risk factors for stroke: People who have risk factors for stroke, such as high blood pressure, high cholesterol, and diabetes, are at higher risk of having a recurrent stroke.
Lack of adherence to post-stroke treatment: People who do not adhere to their post-stroke treatment, such as taking medications, exercising, and eating a healthy diet, are at higher risk of having a recurrent stroke.
stress more stress more stroke .
The symptoms of post-stroke stroke are the same as the symptoms of any stroke.
If you have had a stroke, it is important to work with your doctor to reduce your risk of having a recurrent stroke.
This may involve taking medications, exercising, eating a healthy diet, and managing stress.Other measures.
Here are some tips for preventing post-stroke stroke:
Take all of your medications as prescribed by your doctor.
Exercise regularly. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Eat a healthy diet that is low in saturated and trans fats and high in fruits, vegetables, and whole grains.
Manage stress. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
Get regular medical checkups. See your doctor regularly to monitor your health and manage your risk factors for stroke.
Islamic fasting is the general treatment of great and guaranteed benefit.
fasting
There is growing interest in the potential health benefits of fasting, including for people who have had a stroke.
Some studies have shown that fasting can help to improve brain function,
reduce inflammation, and
protect against neurodegenerative diseases.
One study found that intermittent fasting (IF) improved cognitive function and reduced the risk of stroke in mice.
Another study found that IF protected against brain damage in rats that had a stroke.
Here are some things to keep in mind if you are considering fasting after a stroke:
Fasting can lead to dehydration, which can be dangerous for people who have had a stroke. It is important to drink plenty of fluids while fasting.
Fasting can also lower blood sugar levels, which can be dangerous for people who have diabetes or are taking insulin.
It is important to monitor your blood sugar levels closely while fasting.
Fasting can also interact with medications, so it is important to talk to your doctor before starting any fasting regimen.
If you decide to fast after a stroke, it is important to start slowly and gradually increase the length of your fasts.
It is also important to listen to your body and break your fast if you feel unwell.
Here are some tips for fasting safely:
Start with a short fast, such as 12 hours. Gradually increase the length of your fasts as you become more comfortable.
Listen to your body. If you feel lightheaded, dizzy, or unwell, break your fast.
Stay hydrated. Drink plenty of fluids while fasting. Water is best, but you can also drink unsweetened tea or coffee.
Eat a healthy diet when you break your fast. When you break your fast, it is important to eat a healthy meal that is high in protein and fiber.
fasting islamic in strokes
Fasting is a practice of abstaining from food and drink for a period of time.
It is a common practice in many religions, including Islam.
In Islam, fasting is a pillar of faith and is observed during the month of Ramadan. During Ramadan, Muslims fast from dawn to dusk.
There is some evidence to suggest that fasting may be beneficial for people who have had a stroke.
One study found that fasting improved cognitive function and reduced the risk of stroke in mice. Another study found that fasting protected against brain damage in rats that had a stroke.
Islamic fasting is the general treatment of great and guaranteed benefit.
However, more research is needed to confirm the long-term safety and efficacy of fasting for people who have had a stroke.
Here are some things to keep in mind if you are considering fasting after a stroke:
Fasting can lead to dehydration, which can be dangerous for people who have had a stroke. It is important to drink plenty of fluids while fasting.
Fasting can also lower blood sugar levels, which can be dangerous for people who have diabetes or are taking insulin. It is important to monitor your blood sugar levels closely while fasting.
Fasting can also interact with medications, so it is important to talk to your doctor before starting any fasting regimen.
If you decide to fast after a stroke, it is important to start slowly and gradually increase the length of your fasts. It is also important to listen to your body and break your fast if you feel unwell.
Here are some tips for fasting safely:
Start with a short fast, such as 12 hours. Gradually increase the length of your fasts as you become more comfortable.
Listen to your body. If you feel lightheaded, dizzy, or unwell, break your fast.
Stay hydrated. Drink plenty of fluids while fasting. Water is best, but you can also drink unsweetened tea or coffee.
Eat a healthy diet when you break your fast. When you break your fast, it is important to eat a healthy meal that is high in protein and fiber.
keywords
stroke, brain attack, Ischemic ,Hemorrhagic, fasting . if .post-stroke stroke, prevention . treatment ,taking medications, exercising, eating a healthy diet, and managing stress.Other measures,
Deep Dive: Stroke, Its Management, and Beyond
This document provides a comprehensive overview of key insights and facts about stroke, drawn from various sources, covering post-stroke quality of life assessment, rehabilitation, modern treatments, nutrition, complications, recovery stories, and patients’ rights and available services.
1. Quality of Life Assessment for Post-Stroke Patients with Vertigo:
that most post-stroke patients with vertigo have a moderate quality of life, with a small percentage experiencing poor quality.
The study recommended identifying and modifying factors affecting quality of life to improve early diagnosis and support patients through rehabilitation programs.
It emphasized developing effective compensatory strategies to restore sensory integration and balance.
The World Health Organization defines quality of life as individuals’ perception of their position in life within the context of their culture, values, goals, and expectations.
Vertigo, a common post-stroke symptom, is closely linked to balance loss and increased fall risk, negatively impacting quality of life.
The study highlighted the theoretical importance of addressing post-stroke effects on bodily functions, particularly balance disorders and vertigo, which complicate daily activities.
Methodology: The study included 40 post-stroke vertigo patients at Tishreen University Hospital, using a questionnaire (European Quality of Life 5 Dimensions - EQ-5D) to assess general quality of life and collect demographic data.
Results: Significant differences in quality of life were observed based on age and family size, with better outcomes in the 46-57 age group and those with smaller families (3-5 members).
Chronic disabilities, especially in routine activities, were shown to impact quality of life, with balance and motor coordination issues limiting independence.
The study concluded the need for early intervention, appropriate care, and tailored educational and rehabilitation programs for stroke patients.
2. Post-Stroke Rehabilitation:
Rehabilitation aims to help patients regain lost skills, improve movement, speech, strength, daily living abilities, independence, and quality of life.
Research shows better outcomes for those in intensive rehabilitation programs.
Rehabilitation involves targeted, repetitive activities based on the affected body part or ability.
It includes physical activities like motor skill exercises, constraint-induced therapy, and range-of-motion treatments.
Technological aids such as functional electrical stimulation, robotics, wireless technology, and virtual reality may be used.
Cognitive and psychological activities address cognitive impairments, communication, psychological evaluation, and medication.
Rehabilitation typically begins within 24-48 hours of a stroke during hospitalization and may continue for months or years depending on stroke severity and complications.
It occurs in various settings, including inpatient/outpatient rehabilitation units, skilled nursing facilities, and home-based programs.
A multidisciplinary team, including physicians, rehabilitation nurses, physical and occupational therapists, speech-language pathologists, social workers, psychologists, and vocational counselors, is involved.
Outcomes depend on physical, emotional, social, and therapeutic factors.
3. Modern Advances in Stroke Treatment:
Rapid, accurate diagnosis is the critical first step in stroke management.
Diagnostic services include brain Doppler ultrasound, cerebral angiography, and nerve/muscle testing.
Recent advances include:
Stem Cell Therapy: Aims to regenerate damaged brain tissue, showing improvements in motor and cognitive functions and reduced psychological symptoms.
Repetitive Transcranial Magnetic Stimulation (rTMS): A non-invasive technique using magnetic fields to stimulate brain areas, aiding motor and cognitive recovery and alleviating depression.
Mechanical Thrombectomy: An effective intervention for ischemic stroke, removing blood clots blocking cerebral arteries.
Advanced Medications: Anticoagulants (e.g., Apixaban) and clot-dissolving drugs (e.g., Tenecteplase) improve recovery and reduce long-term complications.
Modern rehabilitation techniques include functional electrical stimulation, robotic-assisted therapy, virtual reality, and transcranial magnetic stimulation.
A comprehensive approach combining rapid diagnosis, innovative treatments, and effective rehabilitation can transform stroke care outcomes.
4. Nutrition After Stroke:
A healthy diet and regular exercise are vital for recovery.
Patients with swallowing difficulties may require softer foods and thicker liquids.
General healthy eating recommendations include consuming whole grains, fruits, vegetables, adequate water, and a diet low in saturated fats, sugar, and salt.
Daily exercise is crucial, with home exercise programs advised by the rehabilitation team.
Maintaining a healthy weight is important, with BMI monitoring by a physician.
Avoid high-sodium foods to reduce sodium intake.
Reading food labels helps make healthier choices.
Dietary group recommendations outline preferred and limited/avoided options for dairy, protein, fruits, vegetables, grains, and more.
5. Stroke Complications:
Stroke leads to complications affecting patients’ lives, including speech/expression difficulties, swallowing issues, memory problems, muscle weakness/spasticity, venous thrombosis, depression/mood swings, chronic headaches, lung/urinary infections, heart clots/arrhythmias, internal bleeding, urinary incontinence, falls/fractures, and seizures.
Prevention involves a balanced diet, regular exercise, avoiding smoking/alcohol, and managing risk factors like hypertension.
6. Psychological Support for Patients:
Long-term physical therapy can lead to loss of hope, making psychological and emotional support essential.
Key support providers include family, treating physicians, physical therapists, and psychologists.
Family: Provides a calm environment, monitors psychological changes, assists with daily tasks, acknowledges progress, and promotes social integration.
Physician: Highlights positive developments and reassures patients about overcoming challenges.
Physical Therapist: Maintains communication, offers support, and encourages patients.
Psychologist: Diagnoses conditions, determines optimal treatments, addresses psychological/social issues, suggests alternatives, and manages treatment side effects.
7. Post-Stroke Management:
Relies on integrated strategies to enhance quality of life and prevent complications.
Includes physical therapy to restore movement, strength, and flexibility; occupational therapy for daily activities; speech therapy for communication and swallowing; medication management to prevent recurrence and control risk factors; psychological/social support via counseling and support groups; long-term rehabilitation; and lifestyle changes like healthy eating, exercise, and quitting smoking.
Requires ongoing follow-up with specialists.
8. Stroke Recovery Stories:
Inspiring stories, like those of Ahmed Al-Amari, Fatima Ahmed, and Sami Jad, highlight the importance of rapid medical intervention, intensive rehabilitation, and family support.
Effective treatments included physical therapy, speech exercises, electrical stimulation, and comprehensive rehabilitation.
Prevention tips: maintain a healthy lifestyle (diet, exercise, no smoking) and regular medical check-ups to detect risk factors early.
9. Rights and Services for Stroke Patients
Patients requiring lifelong medications may receive higher payment caps for drugs.
Disability benefit recipients are exempt from certain healthcare fund service fees.
Recognized rehabilitation patients are entitled to inpatient/community rehabilitation, physical therapy, and home treatment units.
Those affected post-retirement may receive nursing and mobility benefits.
Work-related strokes qualify for occupational injury benefits.
Patients with a medical disability of 89% or higher may receive income tax exemptions.
Discounts on purchase taxes, approval fees, and municipal taxes (Arnona) are available for recognized disabled individuals.
Those with mobility limitations may receive housing adaptation assistance, vocational rehabilitation, and community support services.
Conclusion:
Managing stroke requires a holistic approach encompassing accurate medical assessment, timely acute-phase treatment, intensive and ongoing rehabilitation, psychological and social support, proper nutrition, lifestyle adjustments, and awareness of patients’ rights and services.
Advances in treatment, diagnosis, and rehabilitation offer hope for improved outcomes, reduced disability, and enhanced quality of life for patients and their families.
Deep Dive: Frequently Asked Questions About Stroke and Its Management
What is a stroke, and what are its main types?
A stroke occurs when blood flow to the brain is disrupted, causing nerve cell damage. The two main types are:
Ischemic Stroke: The most common, caused by a blockage in blood vessels preventing blood from reaching part of the brain.
Hemorrhagic Stroke: Results from a ruptured blood vessel in the brain, leading to bleeding.
What symptoms require immediate medical attention when a stroke is suspected?
Key symptoms include facial drooping, arm weakness, and speech difficulties. Even if these symptoms are temporary (as in a transient ischemic attack), immediate emergency contact is critical, as the risk of a full stroke increases in the days or weeks following.
What are the immediate treatment options for ischemic stroke?
The goal of urgent treatment is to restore blood flow to the brain quickly. Options include:
Intravenous Medications: Clot-dissolving drugs like tissue plasminogen activator, administered within 4.5 hours of symptom onset.
Endovascular Interventions: Delivering medications directly to the brain or mechanically removing the clot using a catheter.
What is the role of rehabilitation after a stroke, and what does it involve?
Post-stroke rehabilitation is a comprehensive program to help patients regain lost skills and improve quality of life. It includes:
Physical Therapy: To restore movement, balance, and strength.
Occupational Therapy: To recover the ability to perform daily activities.
Speech and Language Therapy: To enhance communication and swallowing.
Psychological and Social Support: To help patients adapt to changes.
Rehabilitation typically begins in the hospital once the patient stabilizes and may continue for months or years.
How do diet and exercise impact recovery and prevention after a stroke?
Diet: A balanced diet low in saturated fats and sodium, and rich in fiber, fruits, and vegetables, helps control risk factors like high blood pressure and cholesterol. Patients with swallowing difficulties may need modified food textures or liquids under specialist supervision.
Exercise: Regular physical activity aids in regaining strength, flexibility, and balance, and reduces the risk of recurrent strokes. Daily tailored exercise programs are essential.
What are some potential complications of a stroke, and how are they managed?
Complications may include speech/swallowing difficulties, memory issues, muscle weakness/spasticity, depression, and increased risks of venous thrombosis or infections. Management requires a multidisciplinary team providing:
Targeted exercises.
Medications to control symptoms.
Compensatory strategies to improve function.
What are the latest advancements in stroke treatment?
Recent advancements include:
Stem Cell Therapy: To regenerate damaged brain tissue.
Repetitive Transcranial Magnetic Stimulation (rTMS): To enhance motor and cognitive functions.
Mechanical Thrombectomy: For precise clot removal.
Advanced Medications: More effective anticoagulants and clot-dissolving drugs.
Diagnostic Services: Brain Doppler ultrasound and cerebral angiography for rapid, accurate diagnosis.
What is the critical role of psychological and social support in stroke recovery?
Psychological and social support is vital for overcoming emotional challenges like depression, anxiety, and feelings of helplessness. It involves:
Support from family and friends to boost confidence and social integration.
Contributions from psychologists and support groups to improve emotional well-being.
Encouraging patients to achieve small goals and celebrating progress, which enhances rehabilitation commitment and overall quality of life.