weight loss injection : Semaglutide : Mounjaro : Saxenda etc.
Discover how medications like Saxenda and Ozempic, containing semaglutide, aid in weight loss and managing type 2 diabetes. Learn about obesity management, insulin sensitivity, and effective weight loss strategies for better metabolic health.
GENERAL
Dr Hassan Al Warraqi
4/25/2024
Manage Obesity and Diabetes
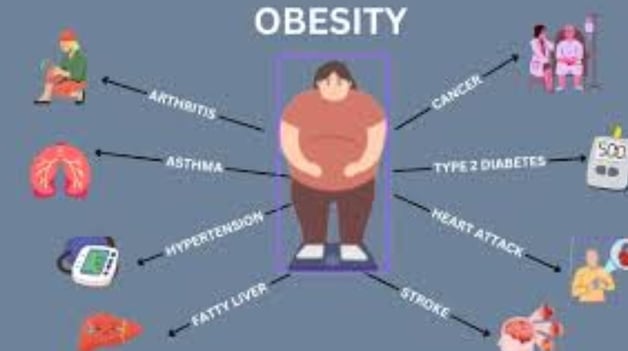
obesity
is a medical condition in which excess body fat accumulates to such an extent that it may have a negative impact on health
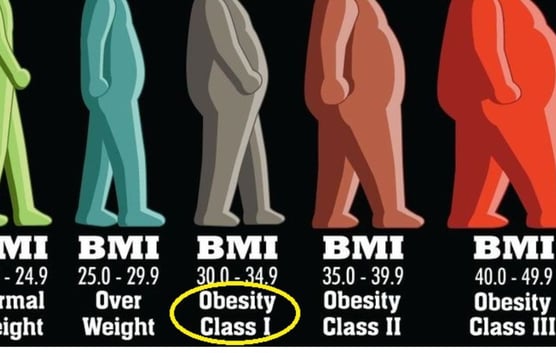
People are considered obese if their body mass index (BMI) is 30 or more
BMI is a measurement that uses your height and weight to estimate your body fat percentage
Main causes of obesity:
Unhealthy diet: Consuming too many calories from sugary drinks, processed foods, and unhealthy fats can lead to weight gain over time
Lack of physical activity: A sedentary lifestyle contributes to obesity. Regular physical activity helps burn calories and maintain a healthy weight
Genetics: Some people are more genetically predisposed to obesity than others
This does not mean that genes determine your fate
You can still make healthy lifestyle choices to reduce your risks
Certain medical conditions: Certain medical conditions, such as Cushing's syndrome and hypothyroidism, can also lead to weight gain
Medications: Some medications can cause weight gain as a side effect.
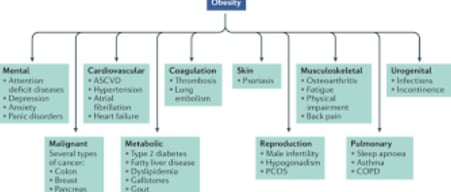
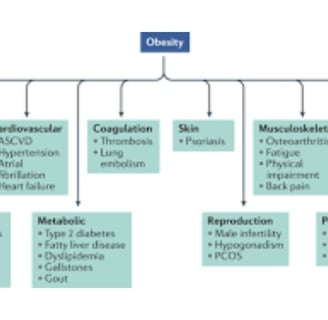
Obesity increases the risk of developing a number of health problems
Type 2 diabetes
My heart disease
Apoplexy
high blood pressure
Sleep Apnea
Some types of cancer
Osteoporosis
Fatty liver disease
Kidney disease
Stress management: Stress can lead to increased appetite and fat storage, so try to find healthy ways to manage stress
Saxenda
GLP-1 is used to treat type 2 diabetes and for weight loss in obese or overweight adults with weight-related diseases.
It works by increasing insulin secretion and suppressing glucagon secretion
Which helps lower blood sugar levels and make you feel full longer
Uzbek
GLP-1 is also used to treat type 2 diabetes and for weight loss in obese or overweight adults with weight-related diseases.
Ozempic works similarly to Saxenda, but may have a stronger effect on lowering blood sugar levels
Mongaro:
Dual action acts on both the GLP-1 receptor and the glucagon-like peptide (GLP-1r) receptor.
It was recently approved to treat type 2 diabetes in adults
It has also shown effectiveness for weight loss in people who are obese or overweight
Monjaro works by increasing insulin secretion and suppressing glucagon secretion
In addition to reducing appetite
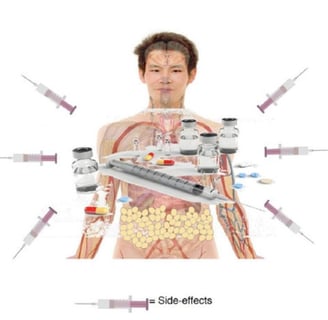
All of these medications are given by subcutaneous injection
It may not be suitable for everyone, especially for those with certain medical conditions
Common side effects
Nausea, vomiting, diarrhea, stomach pain,
loss of appetite, constipation, headache, dizziness, fatigue, pancreatitis.
Serious allergic reactions
Gallstones
These medications can increase the risk of severely low blood sugar levels (hypoglycemia) during fasting
This may make it difficult for you to eat large meals or eat often, which may make fasting more difficult
Fasting as a treatment for obesity
While fasting may help with weight loss, it is not a magic or sustainable long-term solution to obesity
Here are some mechanisms through which fasting may help with weight loss:
Reducing calories: naturally, which leads to a shortage of calories, which enhances the process of burning fat in the body.
Improving insulin sensitivity: This makes the body more effective in using insulin to regulate blood sugar levels, which may help reduce fat storage
Promoting fat burning: which leads to the breakdown of fat stored in the body
Increased levels of fat burning hormones: norepinephrine (adrenaline) and cortisol, which enhances the fat burning process.
Fasting may not be suitable for everyone: diabetes, kidney disease, or eating disorders
Weight loss results may vary: The amount of weight you lose depends on the duration of the fast and other factors such as your diet and activity level.
may experience side effects while fasting, such as hunger, headache, and fatigue
It is important to re-feed slowly: after the end of the fasting period, to avoid digestive system upset
Overall, fasting can be a useful tool for weight loss, but it's important to use it wisely
In addition to fasting
Healthy diet: Eat a diet rich in fruits, vegetables, whole grains, and lean proteins
Exercise regularly: Make sure to do at least 30 minutes of moderate physical activity most days of the week
Get enough sleep: Adequate sleep helps regulate hormones that control appetite and metabolism
Keywords:
Saxenda, Ozambik, Mongar, semaglutide, obesity, diabetes, fasting, intermittent fasting, insulin sensitivity, obesity, weight loss,Nausea, vomiting, diarrhea, stomach pain, loss of appetite, constipation, headache, dizziness, fatigue, pancreatitis,Serious allergic reactions,Gallstones
Understanding Obesity and Type 2 Diabetes: A Comprehensive Guide
This course explores the critical link between obesity and type 2 diabetes, covering diagnostic criteria, metabolic impacts, and evidence-based strategies for prevention and management.
1. Diagnosing Obesity: BMI and Waist Circumference Guidelines
Body Mass Index (BMI):
Primary Tool: BMI estimates body fat and categorizes obesity.
General thresholds: Obesity (BMI ≥30), overweight (BMI 25–29.9).
Asian populations: Lower thresholds due to higher body fat percentages (overweight ≥23, class I obesity ≥27.5, class II ≥32.5, class III ≥37.5).
Waist Circumference:
Visceral Fat Indicator: Measures abdominal obesity linked to cardiometabolic risks.
U.S. thresholds: ≥35 inches (women), ≥40 inches (men).
Asia thresholds: ≥31 inches (women), ≥33 inches (men).
Annual Screening:
Calculate BMI yearly; consider muscle mass, hydration, and sarcopenia during evaluations.
2. Obesity, Insulin Resistance, and Diabetes Risk
Key Connection: 90% of type 2 diabetes cases involve overweight/obesity.
Mechanisms:
Insulin Resistance: Excess abdominal fat releases hormones disrupting insulin function.
Chronic Inflammation: Low-grade inflammation exacerbates metabolic dysfunction.
Weight Loss Challenges: Insulin resistance and diabetes medications (e.g., sulfonylureas, insulin) can hinder weight loss.
3. Weight Management Strategies for Diabetics and Non-Diabetics
Lifestyle Modifications:
Dietary Plans:
Caloric Deficit: 1,200–1,500 kcal/day (women), 1,500–1,800 kcal/day (men).
Focus: Whole foods, fiber-rich diets (e.g., Mediterranean, DASH).
Exercise: 150+ minutes/week of moderate activity + strength training.
Behavioral Support: Self-monitoring, Acceptance and Commitment Therapy (ACT), and community programs (e.g., National DPP).
Pharmacological Interventions:
Weight-Loss Medications:
Indications: BMI ≥30 (≥25 for Asians) or BMI ≥27 (≥23 for Asians) with comorbidities.
Preferred Options: GLP-1 agonists (semaglutide, liraglutide), metformin, orlistat.
Avoid: Insulin, sulfonylureas, and thiazolidinediones due to weight gain risks.
Bariatric Surgery:
Candidates: BMI ≥40 or ≥35 with comorbidities (e.g., diabetes, hypertension).
Procedures: Gastric bypass, sleeve gastrectomy, or adjustable banding.
Outcomes: Improved insulin sensitivity, potential diabetes remission.
4. Early Detection and Risk Factor Management
Prediabetes Indicators:
A1C 5.7–6.4%, fasting glucose 100–125 mg/dL, or post-glucose levels 140–199 mg/dL.
Progression: Up to 50% of prediabetics develop diabetes within 5 years.
Risk Factors:
Obesity, inactivity, family history, ethnicity (e.g., African American, Asian), and conditions like PCOS.
Screening Importance:
Early detection of prediabetes/diabetes enables timely lifestyle interventions.
5. Clinical Best Practices and Patient Communication
5A’s Model for Weight Counseling:
Assess: Obesity status and patient readiness.
Advise: Link weight loss to reduced diabetes/cardiovascular risks.
Agree: Set realistic goals (e.g., 5% weight loss in 6 months).
Assist: Provide resources (dietitians, programs).
Arrange Follow-Up: Monitor progress and adjust plans.
Avoiding Bias:
Use non-stigmatizing language; address medications that promote weight gain (e.g., steroids, antipsychotics).
6. Additional Influences on Obesity and Metabolism
Environmental Factors: Food access, walkability, cultural norms.
Genetics: Impacts fat storage, appetite regulation, and metabolic efficiency.
Intermittent Fasting: May aid weight loss but risks for diabetics (hypoglycemia, fatigue).
Conclusion
Obesity and type 2 diabetes are interconnected epidemics requiring personalized, multidisciplinary care. Combining lifestyle changes, pharmacotherapy, and surgery—along with early screening and empathetic patient communication—can mitigate risks and improve long-term health outcomes.
SEO Keywords: Obesity and type 2 diabetes, BMI thresholds, waist circumference, GLP-1 agonists, insulin resistance, bariatric surgery, prediabetes management, weight loss strategies, National DPP, metabolic health.
FAQS frequently asked questions
How is obesity diagnosed and its associated health risks assessed?
Obesity has traditionally been diagnosed using body mass index (BMI).
However, recent guidelines recommend assessing metabolic health in addition to BMI.
Adults should be screened annually using BMI.
For individuals with a BMI ≥ 25 kg/m² (≥ 23 kg/m² for Asian ethnicity), clinicians should evaluate excess fat, taking into account factors such as muscle mass, hydration status, edema, and sarcopenia.
For those with a BMI ≥ 25 kg/m² but < 35 kg/m², waist circumference measurement is recommended to further stratify risk.
In the United States, a waist circumference ≥ 88 cm (35 inches) for women and ≥ 102 cm (40 inches) for men is considered an indicator of abdominal obesity and an increased risk of cardiometabolic disease.
There are specific waist circumference values that increase risk in Asian populations.
What is the importance of lifestyle changes in weight management and type 2 diabetes prevention?
Lifestyle modifications are the cornerstone of weight management and type 2 diabetes prevention.
A weight loss of 5-7% of body weight aims to achieve significant health benefits, including a 58% reduction in diabetes risk, as outlined by the National Diabetes Prevention Program (DPP).
Recommendations include achieving at least 150 minutes of moderate-intensity physical activity per week, following a balanced diet low in calories and fat, increasing fiber intake, and reducing complex carbohydrate intake if diabetes or insulin resistance is present.
Self-monitoring of weight, physical activity, and dietary intake are important tools for weight loss and maintenance.
What drug treatment options are available for weight loss and type 2 diabetes management?
Several medications are approved for long-term weight loss, often used in conjunction with lifestyle modifications.
These medications include orlistat, lorcaserin, phentermine/topiramate, naltrexone/bupropion, liraglutide, semaglutide, and tirzepatide.
These medications work by:They work by various mechanisms, such as inhibiting fat absorption, suppressing appetite, or increasing satiety, and may lead to significant weight loss and improved glycemic control.
In addition, physicians may consider using glucose-lowering medications that are weight-neutral or promote weight loss in patients with type 2 diabetes and obesity, such as metformin, pramlintide, glucagon-like peptide 1 (GLP-1) receptor agonists, dipeptidyl peptidase 4 (DPP-4) inhibitors, and sodium-glucose cotransporter 2 (SGLT2) inhibitors.
What is the role of glucagon-like peptide 1 (GLP-1) receptor agonists in weight management and diabetes?
GLP-1 receptor agonists were originally designed to manage blood sugar levels in patients with type 2 diabetes.
However, they have also been shown to be effective in promoting weight loss and increasing insulin sensitivity.
These medications work by lowering blood sugar and hemoglobin A1c levels, leading to weight loss through various mechanisms, including slowing gastric emptying, increasing satiety, and reducing appetite.
Some GLP-1 analogues have been approved specifically for weight loss, such as semaglutide (Wegovy) and liraglutide (Saxenda).
These medications can be administered orally or by injection.
What are the bariatric surgery options, and how do they contribute to the treatment of type 2 diabetes?
Bariatric surgery is a treatment option for obese individuals who have not achieved their weight loss goals through lifestyle modifications and drug therapy, or those with weight-related complications such as uncontrolled type 2 diabetes.
Common surgical procedures include
Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (VSG), laparoscopic adjustable gastric banding (LAGB), and biliopancreatic diversion (BPD).
These surgeries work by altering the anatomy of the gastrointestinal tract, leading to early satiety, reducing the absorption surface area, and modifying hormones involved in glucose regulation.
Bariatric surgery is often referred to as metabolic surgery due to its significant impact on blood sugar control and, in many cases, can lead to remission of type 2 diabetes.
How can healthcare professionals communicate effectively with patients about weight management?
Physicians should approach weight management discussions sensitively and avoid judgment, as studies have shown that weight-related biases can negatively impact weight loss behaviors and health outcomes.
It is essential to agree on realistic and measurable weight loss goals with patients, provide support and resources, and regularly monitor progress.
What are the various factors that contribute to obesity and type 2 diabetes?
A variety of factors interact to contribute to the development of obesity and type 2 diabetes.
These factors include unhealthy dietary choices, lack of physical activity, genetic factors (including a genetic predisposition to obesity and insulin resistance), underlying health conditions, certain medications, stress levels, the built environment (such as access to healthy foods and places to exercise), and cultural norms.
Obesity, particularly excess abdominal fat, often leads to insulin resistance and chronic low-grade inflammation, two key mechanisms in the development of type 2 diabetes.
What is the role of blood glucose monitoring in diabetes management?
Regular blood glucose monitoring is critical for effective diabetes management.
Hemoglobin A1c, fasting plasma glucose (FPG), random plasma glucose (RPG), and oral glucose tolerance test (OGTT) tests allow for the diagnosis of diabetes and prediabetes.
For individuals with diabetes, regular self-monitoring of blood glucose levels helps inform decisions about diet, physical activity, and medication.
The A1c test, which measures average blood sugar levels over 2-3 months, helps assess long-term diabetes control.
Identifying prediabetes can help individuals take steps to change their lifestyle and prevent the development of type 2 diabetes.