Voluntary Fasting for Arrhythmia: Benefits & Risks
Explore the benefits of voluntary fasting for arrhythmia, including its effects on atrial fibrillation and ventricular tachycardia. Learn about health precautions, nutrition, hydration, and medication timing to ensure a safe fasting experience.
CARDIOVASCULAR
Dr Hassan Al Warraqi
12/23/202411 min read


Voluntary Fasting for Arrhythmia: Benefits & Risks
Voluntary Islamic Fasting for Arrhythmia or Dysrhythmia
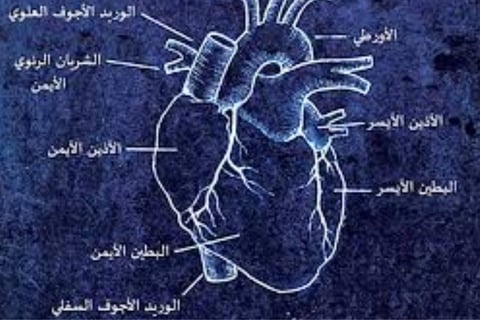
Types of Arrhythmias
Here is an overview of the most common types of arrhythmias:
Atrial Fibrillation (AFib):
Disordered electrical signals in the heart lead to a rapid and irregular heartbeat. AFib episodes may resolve on their own or require medical intervention. This condition is linked to an increased risk of stroke.Atrial Flutter:
Similar to AFib, atrial flutter causes rapid heartbeats but follows a more organized rhythm. It also increases the likelihood of stroke.Supraventricular Tachycardia (SVT):
This broad category covers irregular heartbeats that originate above the ventricles (lower heart chambers). SVT episodes typically cause sudden, pounding heartbeats that begin and end abruptly.Ventricular Fibrillation (VFib):
Chaotic electrical signals cause the ventricles to quiver rather than contract effectively. VFib is a life-threatening emergency requiring immediate restoration of normal heart rhythm. It is often associated with underlying heart disease or trauma.Ventricular Tachycardia (VT):
A rapid, irregular heart rhythm starting in the ventricles that prevents proper blood flow. In healthy hearts, VT may not be serious, but in those with heart disease, it can be a critical emergency.
The Impact of Fasting on Arrhythmias
Fasting, such as Islamic Sunnah fasts (e.g., Mondays, Thursdays, or Ayyam al-Beed) or other voluntary fasting practices such as david fast day after the other or fast every day except friday, , can influence arrhythmias depending on the individual's condition, the type of arrhythmia, and how the fast is managed.
Potential Benefits of Fasting for Arrhythmia
Improved Metabolic Health:
Enhances insulin sensitivity and reduces inflammation, indirectly benefiting heart rhythm.
Lowers oxidative stress, which may stabilize heart electrical activity.
Weight Management:
Promotes weight loss, reducing cardiovascular strain and potential arrhythmia triggers.
Reduced AFib Risk:
Regular fasting may improve metabolic markers, such as blood sugar and cholesterol, helping prevent AFib triggers like high blood pressure and obesity.
Spiritual and Emotional Well-being:
Fasting fosters mindfulness and spiritual focus, which can reduce stress and anxiety—factors that exacerbate arrhythmias.
Potential Risks of Fasting for Arrhythmia
Electrolyte Imbalance:
Fasting may deplete essential electrolytes like potassium, magnesium, and sodium, crucial for maintaining stable heart rhythms.
Dehydration:
Prolonged fasting, especially in hot climates, can increase dehydration risk, leading to palpitations or arrhythmias.
Blood Sugar Fluctuations:
Hypoglycemia from extended fasting can stress the heart and trigger arrhythmias.
Medication Challenges:
Arrhythmia medications, such as beta-blockers or anticoagulants, require consistent dosing, which fasting schedules may disrupt.
Guidelines for Safe Fasting with Arrhythmia
Consult Your Doctor:
Always discuss fasting plans with a healthcare provider to evaluate risks and adjust medications as needed.
Stay Hydrated:
Drink plenty of water during non-fasting hours and include hydrating foods like soups, fruits, and yogurt in Suhoor (pre-dawn meal) and Iftar (breaking the fast).
Maintain Balanced Nutrition:
Focus on nutrient-rich foods, especially those high in potassium and magnesium, such as bananas, dates, leafy greens, and nuts.
Limit salt, sugar, and caffeine intake to avoid dehydration and heart strain.
Ease Into Fasting:
Begin with shorter fasts to observe how your body responds before committing to regular voluntary fasts.
Monitor Symptoms:
Watch for warning signs such as dizziness, chest pain, severe palpitations, or fainting. Break the fast immediately and seek medical advice if symptoms occur.
Prioritize Suhoor:
Never skip Suhoor to maintain stable energy and blood sugar levels throughout the fasting day.
Adjust Medication Timing:
Work with your doctor to synchronize medication schedules with fasting hours to maintain drug efficacy and safety.
Spiritual Perspective
Islamic fasting is an act of worship, but health and well-being are prioritized in Islam.
The Qur'an emphasizes the importance of preserving life:
"And do not kill yourselves [or one another]. Indeed, Allah is to you ever Merciful." (Surah An-Nisa: 4:29)
"ولا تقتلوا أنفسكم إن الله كان بكم رحيما" (سورة النساء: 4:29)
If fasting poses health risks, alternative acts of devotion, such as charity or additional prayers, can be performed.
Conclusion
Voluntary Islamic fasting can provide spiritual and physical benefits but requires caution for individuals with arrhythmias or dysrhythmias. Consulting a healthcare provider, maintaining hydration and nutrition, and monitoring symptoms are essential for a safe fasting experience.
keywords
Voluntary Fasting, arrhythmia, atrial fibrillation, ventricular tachycardia, benefits, risks, electrolytes, hydration, nutrition, medication timing, spiritual well-being, health precautions,.
How do different fasting patterns affect different types of heart rhythm disorders?
Different fasting patterns affect different types of heart rhythm disorders in multiple ways, with both potential benefits and risks.
Types of heart rhythm disorders and the effects of fasting on them:
Atrial fibrillation (AFib): Regular fasting may reduce the risk of atrial fibrillation by improving metabolic markers such as blood sugar and cholesterol, which helps prevent triggers such as high blood pressure and obesity. However, it should be noted that fasting may lead to electrolyte imbalance, which may negatively affect the regularity of the heartbeat.
Atrial flutter: Similar to atrial fibrillation, atrial flutter causes a rapid and regular heartbeat, and fasting increases the risk of stroke.
Supraventricular tachycardia (SVT): This type includes heart rhythm disturbances that originate above the ventricles, and usually cause rapid and sudden heartbeats. Fasting may worsen this condition due to low blood sugar and stress on the heart.
Ventricular fibrillation (VFib): This is a life-threatening emergency condition in which the ventricles quiver instead of contracting effectively, and is often associated with heart disease or trauma. Fasting may increase the risk of this condition due to electrolyte imbalance and dehydration.
Ventricular tachycardia (VT): This is a heart rhythm disorder that begins in the ventricles. It may not be dangerous in healthy hearts, but it can be an emergency in the presence of heart disease. Fasting may affect this condition in a similar way to ventricular fibrillation.
Potential benefits of fasting:
Improved metabolic health: Fasting enhances insulin sensitivity and reduces inflammation, which indirectly benefits heart rhythm.
Reduced oxidative stress: It may help stabilize the heart’s electrical activity.
Weight management: It promotes weight loss, which reduces stress on the heart and potential arrhythmia triggers.
Spiritual and emotional well-being: Fasting enhances spiritual awareness, which reduces stress and anxiety, both of which can exacerbate arrhythmias.
Potential risks of fasting:
Electrolyte imbalance: Fasting may deplete essential electrolytes such as potassium, magnesium, and sodium, which are essential for maintaining a regular heartbeat.
Dehydration: Fasting for long periods, especially in hot climates, can increase the risk of dehydration, leading to palpitations or arrhythmias.
Blood sugar fluctuations: Hypoglycemia resulting from prolonged fasting can strain the heart and trigger arrhythmias.
Medication challenges: Medications for arrhythmias require fixed doses, and fasting can disrupt these doses.
Guidelines for safe fasting with arrhythmias:
Consult your doctor: Always consult your doctor before starting fasting to assess your risks and adjust your medications as needed.
Drink plenty of water: Drink plenty of water during non-fasting hours, and eat hydrating foods at suhoor and iftar.
Maintain a balanced diet: Focus on nutrient-rich foods, especially those rich in potassium and magnesium.
Limit salt, sugar, and caffeine: To avoid dehydration and stress on the heart.
Start with a short fast: To monitor your body’s response before committing to regular fasting.
Monitor symptoms: Symptoms such as dizziness, chest pain, severe palpitations, or fainting should be monitored, and fasting should be broken immediately and medical advice sought if they occur.
Do not miss Suhoor: To maintain stable energy and blood sugar levels throughout the fasting day.
Adjust medication timing: In collaboration with your doctor to maintain the effectiveness and safety of medications.
Conclusion:
Voluntary fasting, such as sunnah fasting or alternate-day fasting, can provide spiritual and physical benefits, but requires caution for individuals with heart rhythm disorders. Consulting a doctor, maintaining hydration and nutrition, and monitoring symptoms are essential for a safe fasting experience.
What are the potential risks and benefits of fasting for overall heart health?
For heart health, fasting can have potential benefits and risks, depending on your individual health status, the type of fasting, and how you manage it.
Potential benefits of fasting for the heart:
Improved metabolic health: Fasting may enhance insulin sensitivity and reduce inflammation, which positively impacts heart rhythm.
Reducing oxidative stress: Fasting may reduce oxidative stress, which can help stabilize the electrical activity of the heart.
Weight management: Fasting helps with weight loss, which reduces stress on the heart and blood vessels, thereby reducing risk factors that cause arrhythmias.
Reducing the risk of atrial fibrillation: Regular fasting may improve metabolic markers such as blood sugar and cholesterol levels, which helps prevent atrial fibrillation triggers such as high blood pressure and obesity.
Spiritual and emotional comfort: Fasting enhances spiritual awareness and focus, which reduces stress and anxiety, two factors that can exacerbate arrhythmias.
Potential risks of fasting on the heart:
Electrolyte imbalance: Fasting may deplete essential electrolytes such as potassium, magnesium, and sodium, which are essential for maintaining a stable heart rhythm.
Dehydration: Prolonged fasting, especially in hot weather, may increase the risk of dehydration, which can lead to palpitations or irregular heartbeats.
Blood sugar fluctuations: May lead to:
Hypoglycemia resulting from prolonged fasting can strain the heart and trigger arrhythmias.
Medication challenges: Heart arrhythmia medications such as beta blockers and anticoagulants require fixed doses, which can be disrupted by the fasting schedule.
Guidelines for safe fasting for patients with arrhythmia:
Consult your doctor: Fasting plans should always be discussed with your healthcare provider to assess risks and adjust medications as needed.
Stay hydrated: Drink plenty of water during non-fasting hours and include hydrating foods such as soup, fruits, and yogurt in suhoor and iftar.
Maintain a balanced diet: Focus on nutrient-rich foods, especially those rich in potassium and magnesium such as bananas, dates, leafy greens, and nuts.
Limit your salt, sugar, and caffeine intake to avoid dehydration and heart stress.
Gradually fast: Start with shorter fasts to monitor your body’s response before committing to regular voluntary fasting.
Monitor symptoms: Pay attention to warning signs such as dizziness, chest pain, severe palpitations, or fainting. Break the fast immediately and seek medical advice if symptoms occur.
Prioritize Suhoor: Do not skip Suhoor to maintain stable energy and blood sugar levels throughout the fasting day.
Adjust medication timing: Work with your doctor to synchronize medication schedules with fasting hours to maintain medication effectiveness and safety.
Spiritual perspective:
Fasting is considered an act of worship in Islam, but health and safety are paramount in Islam. The Holy Quran emphasizes the importance of preserving life. If fasting poses health risks, alternative acts of worship such as charity or extra prayers can be performed.
In general, voluntary fasting can provide spiritual and physical benefits, but caution is required for individuals with arrhythmias. Maintaining hydration, nutrition, and monitoring symptoms are essential for a safe fasting experience.
What are the guidelines for safe fasting for patients with arrhythmias?
Based on sources and conversation history, here are some guidelines for safe fasting for patients with arrhythmia:
Consult your doctor: Always talk to your doctor before starting fasting to assess potential risks and adjust medications if necessary.
Stay hydrated: It is important to drink enough water during the hours of Iftar. You should also eat hydrating foods such as soup, fruits, and yogurt during Suhoor and Iftar.
Dehydration can increase the risk of palpitations and irregular heartbeats, so staying hydrated is crucial.
Balanced nutrition: Focus on eating nutrient-rich foods, especially those containing potassium and magnesium, such as bananas, dates, leafy greens, and nuts. These minerals are important for maintaining a stable heart rhythm.
Reducing salt, sugar, and caffeine: Salt, sugar, and caffeine intake should be reduced to avoid dehydration and stress on the heart1. These substances can negatively affect the body’s balance and increase the risk of arrhythmia.
Gradual fasting: It is best to start with shorter fasting periods to monitor the body’s response before committing to regular fasting.
This allows us to determine the extent of the effect of fasting on the body and avoid any potential complications.
Monitoring symptoms: Attention should be paid to any warning symptoms such as dizziness, chest pain, severe palpitations, or fainting. If any of these symptoms appear, the fast should be broken immediately and medical advice should be sought.
These symptoms may indicate that fasting is negatively affecting the heart, and should be addressed immediately.
Do not miss Suhoor: Be sure to eat Suhoor to ensure that energy and blood sugar levels are stable throughout the fasting period.
Skipping Suhoor can lead to fluctuations in blood sugar, which may affect the heart.
Adjusting medication schedules: Work with your doctor to adjust medication schedules to coincide with iftar hours, to ensure the effectiveness and safety of the medications.
Medications that are taken irregularly may lose their effectiveness and may increase the risk of irregular heartbeats.
Spiritual perspective: It should be taken into account that Islam places great importance on maintaining health and safety, and if fasting poses a health risk, it can be replaced with other acts of worship6. Physical health is an integral part of the Islamic faith, and if fasting causes harm, it is not considered obligatory.
By following these guidelines, individuals with arrhythmia can safely fast while taking the necessary safety precautions.
Spiritual perspective:
Fasting in Islam is an act of worship, but health and safety are paramount in Islam, and the Quran has made clear the importance of preserving life.
If fasting poses health risks, alternative acts of worship such as charity or additional prayers can be performed.
In general, voluntary fasting can provide spiritual and physical benefits, but it requires caution for individuals with arrhythmia. Consulting a physician, maintaining hydration and nutrition, and monitoring symptoms are essential for a safe fasting experience.
How does fasting affect electrolyte balance?
Based on sources and conversation logs, here is how fasting affects electrolyte balance:
Essential electrolyte depletion: Fasting, especially prolonged fasting, can deplete essential electrolytes such as potassium, magnesium, and sodium. These electrolytes are essential for maintaining a stable heart rhythm.
Importance of Electrolytes: These electrolytes play a crucial role in the electrical and muscular functions of the heart, and any imbalance in their levels can lead to heart rhythm problems. For example, potassium is essential for the function of nerve and muscle cells, including the heart muscle, while magnesium helps regulate heartbeat and blood pressure.
Increased risk of irregular heartbeat: A deficiency in these electrolytes can increase the risk of
Irregular heartbeat, especially in individuals who already have heart problems1. This is because electrolytes play a key role in transmitting electrical signals in the heart, and any imbalance in them can lead to disturbances in these signals.
Dehydration and worsening of the imbalance: Dehydration resulting from fasting can worsen electrolyte imbalance, increasing the risk of heart complications1. When the body is dehydrated, electrolyte concentrations in the blood increase, which can lead to serious imbalances.
Recommendations to reduce the risk: It is important to eat foods rich in electrolytes during the hours of breaking the fast to compensate for the loss during fasting.
These foods include bananas, dates, leafy greens, and nuts, which are high in potassium and magnesium. In addition, adequate amounts of water should be drunk to avoid dehydration.
Medical monitoring: Individuals with irregular heartbeats are advised to consult a doctor before fasting, to assess potential risks and adjust medications if necessary.
The doctor may recommend monitoring blood electrolyte levels during fasting, especially if the individual is at high risk.
In short
Fasting can deplete essential electrolytes, which can negatively impact heart health and increase the risk of arrhythmia. Therefore, care must be taken to maintain electrolyte balance through proper nutrition and adequate hydration during Iftar hours, monitoring symptoms, and consulting a doctor when needed.
How can the risks of fasting be reduced for these patients?
Based on sources and conversation logs, the risks of fasting for individuals with arrhythmia can be reduced through several measures:
Consult a doctor: It is essential to consult a doctor before starting fasting to assess risks and adjust medications if necessary.
Stay hydrated: Drink adequate amounts of water during Iftar hours to replace fluids lost during fasting. It is recommended to eat hydrating foods such as soup, fruits, and yogurt during Suhoor and Iftar meals.
Dehydration can increase the risk of palpitations or arrhythmias.
Balanced nutrition: Focus on eating foods rich in nutrients, especially those rich in potassium and magnesium, such as bananas, dates, leafy greens, and nuts.
These elements are essential to maintain electrolyte balance and stabilize heart rhythm.
Limit salt, sugar, and caffeine intake: Reduce salt, sugar, and caffeine intake to avoid dehydration and heart stress.
Graduating fasting: It is recommended to start with shorter fasts to monitor the body’s response before committing to regular voluntary fasting.
Monitor symptoms: Pay attention to warning signs such as dizziness, chest pain, severe palpitations, or fainting. If any of these symptoms occur, break the fast immediately and seek medical advice.
Prioritize Suhoor: Do not skip the Suhoor meal to maintain stable energy and blood sugar levels throughout the day.
Adjust medication timing: Work with your doctor to adjust medication timing to fasting hours to maintain the effectiveness and safety of the medication. It may be necessary to change the timing of medication to avoid any negative interactions with fasting.
Understand the importance of electrolytes: It is important to understand that fasting can lead to depletion of essential electrolytes such as potassium, magnesium, and sodium, which are essential to maintaining stable heart rhythm.
Therefore, you must be careful to compensate for it during the breakfast hours.