Fasting In Tumor Lysis Syndrome
Explore the potential benefits of fasting in managing tumor lysis syndrome (TLS), including reduced metabolic stress and enhanced chemosensitivity. Learn about risks like malnutrition and electrolyte imbalances, and the limited clinical evidence supporting these claims.
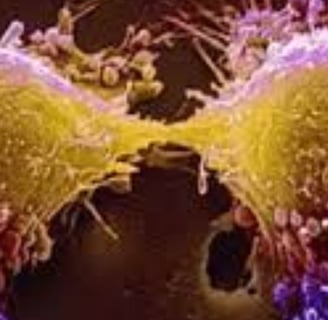
CANCER
Dr Hassan Al Warraqi
12/25/20246 منٹ پڑھیں

Fasting in Tumor Lysis Syndrome
Fasting and Tumor Lysis Syndrome Benefits & Risks
Fasting or fasting-mimicking approaches have been explored in the context of cancer treatment and its side effects,
but their role in prevention and management of Tumor Lysis Syndrome (TLS) remains largely theoretical and not well-established in clinical practice.
Below is an analysis of the potential role of fasting based on current knowledge:
Theoretical Benefits of Fasting in TLS
Reduced Metabolic Load:
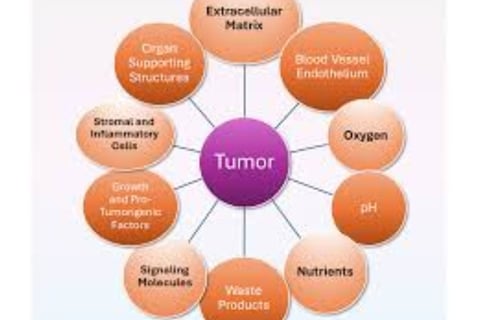
During fasting, the body's metabolic activity shifts to prioritize autophagy and repair mechanisms. This may reduce the metabolic stress associated with the rapid turnover and breakdown of tumor cells.
Fasting may lower serum levels of glucose, insulin, and other nutrients that are crucial for tumor growth, potentially decreasing the overall tumor burden.
Regulation of Uric Acid and Electrolytes:
Fasting has been suggested to modulate purine metabolism, which could theoretically reduce the levels of uric acid released during cell lysis.
Autophagy induced by fasting might help maintain intracellular electrolyte balance, potentially mitigating TLS-associated hyperkalemia and hyperphosphatemia.
Enhancement of Chemosensitivity:
Preclinical studies have suggested that fasting may enhance the efficacy of chemotherapy by making cancer cells more susceptible to treatment while protecting normal cells, possibly reducing the tumor burden and modulating the severity of TLS.
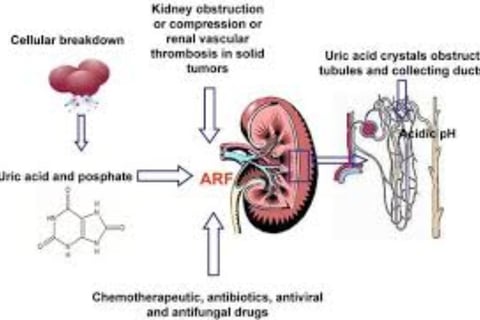
Protection Against Kidney Injury:
Fasting may reduce oxidative stress and inflammation, potentially protecting the kidneys from TLS-related damage.
Challenges and Risks of Fasting in TLS
Risk of Malnutrition:
Cancer patients are often at risk of malnutrition due to the disease or treatment side effects. Prolonged fasting may exacerbate malnutrition, which can weaken overall resilience to therapy.
Electrolyte Imbalances:
Fasting can alter electrolyte levels, and in a TLS-prone setting, this may complicate the management of hyperkalemia, hyperphosphatemia, or hypocalcemia.
Lack of Direct Evidence:
While fasting has shown promise in reducing side effects of cancer therapy in some preclinical and small-scale human studies, no robust evidence directly supports its role in preventing or treating TLS.
Unpredictable Tumor Behavior:
Tumors with a high proliferation rate may not respond uniformly to fasting, and the risk of abrupt cell death with therapy remains.
Current Clinical Recommendations
TLS-Specific Measures Take Precedence:
Proven measures such as hydration, electrolyte monitoring, and pharmacologic interventions (e.g., allopurinol, rasburicase) are the mainstay for TLS prevention and treatment.
Adjunctive Role of Fasting (Under Supervision):
If fasting is considered, it should be implemented cautiously and under strict medical supervision, especially in patients undergoing intensive chemotherapy or with high TLS risk.
Potential Research Area:
While fasting is not part of standard TLS prevention or treatment protocols, it represents a potential area for further clinical research, particularly in terms of its ability to modulate systemic metabolism and improve treatment outcomes.
Conclusion
Fasting shows theoretical potential for mitigating TLS by reducing metabolic stress, modulating nutrient availability, and enhancing treatment response.
However, due to a lack of direct evidence and potential risks, fasting is not recommended as a primary strategy for TLS prevention or treatment at this time.
Standard interventions remain the cornerstone of TLS management. Further research is needed to clarify the role of fasting in this context.
https://emedicine.medscape.com/article/282171-overview
https://www.mdpi.com/2072-6694/16/11/2079
https://pmc.ncbi.nlm.nih.gov/articles/PMC3608686/
https://ezra.com/blog/fasting-and-cancer
https://www.mdpi.com/2673-6357/5/4/31
keywords
Fasting and tumor lysis syndrome (TLS), potential benefits ,include reduced metabolic stress, enhanced chemosensitivity, uric acid regulation, and kidney protection, but clinical evidence is limited, and risks like malnutrition , electrolyte imbalances , .
Frequently asked questions about tumor lysis syndrome (TLS) and the potential role of fasting
What is tumor lysis syndrome (TLS) and what causes it?
Tumor lysis syndrome (TLS) is a serious medical emergency that occurs when a large number of cancer cells die rapidly, releasing their internal contents into the bloodstream.
It usually occurs after the start of cancer treatment such as chemotherapy, targeted therapy, or radiation, especially in cancers with high cell turnover rates, such as hematologic malignancies (such as leukemia and lymphoma).
This rapid cell breakdown releases potassium, phosphate, and uric acid, causing hyperkalemia, hyperphosphatemia, and hyperuricemia, as well as hypocalcemia due to the binding of phosphate to calcium.
These metabolic abnormalities can lead to serious complications such as acute kidney injury, cardiac arrhythmias, seizures, and multiple organ failure.
What are the risk factors that increase the likelihood of developing tumor lysis syndrome?
Tumor-related risk factors include: high tumor load (such as large lymphoma or high white blood cell counts in leukemia), rapid spread or sensitivity to treatment, and certain types of cancer such as Burkitt lymphoma and acute lymphoblastic leukemia (ALL).
Patient-related risk factors include: previous kidney dysfunction, dehydration or poor hydration.
For treatment, risk factors include chemotherapy or intensive targeted therapies, and use of corticosteroids.
How is tumor lysis syndrome diagnosed? What is the difference between laboratory and clinical tumor lysis syndrome?
Tumor lysis syndrome is diagnosed based on the presence of laboratory abnormalities, especially if there are clinical signs.
TLS is classified into: Laboratory tumor lysis syndrome: defined as the presence of at least two abnormalities (hyperuricemia, hyperphosphatemia, hyperkalemia, or hypocalcemia) within 3 days before or 7 days after starting treatment.
Clinical tumor lysis syndrome: is the laboratory tumor lysis syndrome plus clinical complications, such as acute kidney injury, cardiac arrhythmias, or seizures.
How is tumor lysis syndrome managed and treated? What are the preventive measures?
Management of tumor lysis syndrome involves several key aspects:
Prevention: includes intensive intravenous hydration (2-3 L/m2/day) to maintain diuresis, use of medications such as allopurinol (to prevent uric acid formation) and rasburicase (to convert uric acid to the more soluble allanoate), and proactive monitoring and correction of electrolyte imbalances.
Treatment: includes management of electrolyte imbalances, such as calcium gluconate (to protect the heart) and insulin with glucose or potassium binders to treat hyperkalemia, use of phosphate binders or dialysis if hyperphosphatemia is severe, and treatment of hypocalcemia only if it is symptomatic.
In addition, treatment also includes improving hydration, treating acute kidney injury and dialysis if necessary, and aggressively managing cardiac and neurological symptoms such as arrhythmias and seizures.
What is the potential role of fasting in the prevention and treatment of TLS?
The role of fasting in the prevention and treatment of TLS remains theoretical and not well established clinically.
Potential theoretical benefits of fasting include reducing metabolic burden, regulating uric acid and electrolyte levels, enhancing the sensitivity of cancer cells to therapy, and protecting the kidneys from damage.
However, fasting may increase the risk of malnutrition and worsening electrolyte imbalances.
Currently, there is no strong evidence to support the use of fasting as a primary strategy for the prevention or treatment of TLS.
What are the challenges and risks associated with the use of fasting in cases of TLS?
Challenges and risks associated with fasting in TLS include the risk of malnutrition, especially in cancer patients already at risk, and the potential for electrolyte imbalances that may complicate the management of hyperkalemia, hyperphosphatemia, and hypocalcemia.
In addition, there is no direct evidence to support the efficacy of fasting in prevention or treatment, and tumor behavior may be unpredictable when fasting, increasing the risk of sudden cell death with treatment.
Is fasting recommended as part of TLS treatment protocols?
Currently, fasting is not recommended as a major part of TLS prevention or treatment protocols.
Standard measures such as hydration, electrolyte monitoring, and pharmacological interventions are the foundation of TLS management.
If fasting is considered, it should be implemented with caution and under strict medical supervision, especially in patients undergoing intensive chemotherapy or at high risk for TLS.
Fasting is a potential area for further clinical research, but is not currently part of standard treatment protocols.
What is the importance of early diagnosis and appropriate management of tumor lysis syndrome?
Early diagnosis and appropriate management of tumor lysis syndrome are of great importance to significantly improve outcomes.
Delaying treatment can lead to serious complications, including death.
With appropriate preventive measures, tumor lysis syndrome can be largely prevented in at-risk patients.
Therefore, close monitoring and prompt intervention are of paramount importance.