Starvation Diabetes : Fasting-Induced Insulin Resistance
Starvation diabetes is a temporary physiological adaptation that occurs during prolonged fasting or severe calorie restriction. This condition involves the body's reduction of glucose uptake in per...
FASTINGDIABETES
Dr Hassan Al Warraqi
4/22/20256 min read


Starvation Diabetes : Fasting-Induced Insulin Resistance
Fasting-induced insulin resistance, also known as starvation diabetes, is a temporary physiological adaptation during prolonged fasting or severe calorie restriction, where the body reduces glucose uptake in peripheral tissues to prioritize glucose availability for vital organs like the brain.
Voluntary Fasting: Mimicking Starvation Diabetes?
Voluntary fasting practices can induce transient insulin resistance similar to starvation diabetes, but outcomes depend on fasting duration and individual health
Detailed Analysis
1. Mechanism of Fasting-Induced Insulin Resistance
Physiological Adaptation: Prolonged fasting triggers the breakdown of stored fats, releasing free fatty acids that impair insulin signaling, causing insulin resistance in muscles and the liver.
This preserves glucose for brain function.
Liver’s Role: The liver ramps up gluconeogenesis, producing glucose from non-carbohydrate sources (e.g., amino acids), which can elevate blood sugar despite fasting.
Hormonal Shifts: Stress hormones (cortisol, glucagon, epinephrine) rise, promoting glycogenolysis and gluconeogenesis, while insulin levels drop, further reducing glucose uptake in peripheral tissues.
Ketone Production: As fasting persists, the body shifts to ketogenesis, producing ketones from fats as an alternative energy source, reducing glucose dependence.
2. Short-Term vs. Prolonged Fasting
Short-Term Fasting (12–24 hours):
Generally safe for healthy individuals, causing mild, transient insulin resistance.
Promotes fat-burning and ketone production, stabilizing blood glucose.
May enhance insulin sensitivity long-term by reducing insulin levels and aiding weight loss.
Prolonged Fasting (24–72+ hours):
Triggers more pronounced insulin resistance after 48 hours due to glycogen depletion and increased gluconeogenesis.
Elevates blood glucose and ketones, resembling starvation diabetes.
Healthy individuals typically tolerate this, with insulin sensitivity often improving post-fast.
Extreme Fasting/Starvation (days to weeks):
Exacerbates insulin resistance, increases stress hormones, and breaks down muscle for gluconeogenesis.
Reverses with refeeding, but risks complications like refeeding syndrome.
3. Risk Factors
Unsupervised Fasting: Dangerous for individuals with diabetes or obesity, as it may cause erratic blood sugar levels or disrupt medication needs.
Nutritional Deficiencies: Lack of fiber, protein, or micronutrients during eating windows can worsen insulin resistance.
Intense Exercise During Fasting: Depletes glucose reserves, raising the risk of hypoglycemia and compensatory insulin resistance.
4. Symptoms and Potential Complications
Signs of Insulin Resistance
Elevated fasting blood glucose (>100 mg/dL).
Increased waist circumference, indicating visceral fat accumulation.
Complications
Potential progression to prediabetes or type 2 diabetes if fasting is mismanaged.
Increased cardiovascular risk due to elevated LDL cholesterol or chronic inflammation.
5. Safe Fasting Practices
Medical Supervision: Essential for adjusting medications (e.g., insulin) and monitoring high-risk individuals.
Balanced Nutrition: Prioritize fiber-rich foods (e.g., whole grains) and lean proteins during eating windows to support metabolic health.
Hydration: Drink water, unsweetened teas, or calorie-free electrolyte solutions to prevent dehydration, which can concentrate blood glucose.
Regular Monitoring: Check blood sugar frequently, especially if symptoms like dizziness, sweating, or fatigue occur.
Gradual Approach: Start with shorter fasts (e.g., 16:8 intermittent fasting) to build tolerance and minimize metabolic stress.
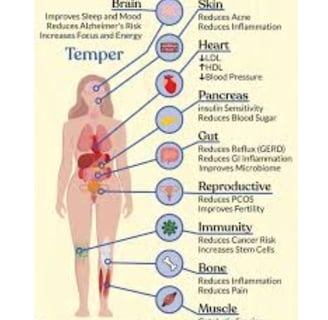
Benefits of Voluntary Fasting
Metabolic Flexibility: Enhances the body’s ability to switch between glucose and fat metabolism, potentially improving long-term insulin sensitivity.
Autophagy: May promote cellular repair, though human evidence is limited.
Weight Loss: Reduces calorie intake, aiding fat loss and improving insulin sensitivity in overweight individuals.
Risks and Considerations
Pre-existing Conditions: Individuals with diabetes, hypoglycemia, or metabolic disorders face higher risks and should consult a doctor.
Refeeding Syndrome: Rapid refeeding after prolonged fasting can cause electrolyte imbalances, particularly in malnourished individuals.
Individual Variability: Age, sex, fitness, and baseline health influence fasting outcomes; women may experience hormonal disruptions from extended fasts.
Practical Tips for Voluntary Fasting
Start Gradually: Begin with shorter fasts to adapt to metabolic changes.
Stay Hydrated: Maintain fluid and electrolyte balance to support metabolism.
Monitor Symptoms: Break the fast if dizziness, extreme fatigue, or confusion occurs.
Break Fasts Wisely: Reintroduce small, nutrient-dense meals to avoid digestive issues or glucose spikes.
Personalize Approach: Adjust fasting based on individual response, as it’s not suitable for everyone.
Scientific Context
Research (e.g., Cahill et al., 1970) shows insulin resistance peaks around 3–5 days of fasting but reverses with refeeding. Intermittent fasting studies (e.g., Halberg et al., 2005) suggest short-term fasting improves insulin sensitivity in healthy individuals, while prolonged fasting transiently mimics starvation diabetes. Long-term fasting (>7 days) data is scarce due to ethical limitations.
Conclusion
Intermittent fasting can enhance insulin sensitivity and support weight management, but prolonged fasting may induce temporary insulin resistance as a survival mechanism.
High-risk individuals, such as those with diabetes or obesity, require medical supervision to avoid complications.
Tailored guidance, gradual adaptation, and careful monitoring are crucial for balancing fasting’s metabolic benefits and risks.
If you’re considering fasting or have specific health concerns, consult a healthcare provider.
Keywords
Fasting-induced insulin resistance, starvation diabetes, voluntary fasting, gluconeogenesis, ketogenesis, glucose sparing, insulin sensitivity, metabolic flexibility, autophagy, refeeding syndrome.
FAQs: Voluntary Fasting and Starvation Diabetes
1. What is starvation diabetes, and how does it relate to voluntary fasting?
Answer:
Starvation diabetes (fasting-induced insulin resistance) is a temporary state where prolonged fasting triggers insulin resistance to conserve glucose for vital organs like the brain.
Voluntary fasting (e.g., intermittent fasting) can mimic this effect, depending on duration and individual health.
Short-term fasting is generally safe, but prolonged fasting (>48 hours) may induce transient insulin resistance similar to starvation diabetes.
2. Does voluntary fasting always lead to insulin resistance?
Answer:
No. Short-term fasting (12–24 hours) often improves insulin sensitivity by promoting fat-burning and lowering insulin levels.
Prolonged fasting (>24–48 hours) may cause temporary insulin resistance as the body shifts to gluconeogenesis and prioritizes glucose for the brain.
This resistance typically reverses once normal eating resumes.
3. What happens to blood sugar during voluntary fasting?
Answer:
Short-term fasting (12–24 hours): Blood glucose stabilizes or slightly rises as the liver releases stored glycogen.
Prolonged fasting (>48 hours): Blood glucose may paradoxically increase due to gluconeogenesis, mimicking starvation diabetes.
Ketones: After ~48 hours, ketones become a primary energy source, reducing glucose dependence.
4. Can voluntary fasting worsen diabetes or prediabetes?
Answer:
For healthy individuals, fasting is generally safe and may improve metabolic health.
However, people with diabetes or prediabetes risk dangerous glucose fluctuations or medication mismatches.
Always consult a doctor before fasting if you have metabolic conditions.
5. What are the benefits of voluntary fasting?
Answer:
Improved insulin sensitivity (short-term fasting).
Weight loss, reducing obesity-related insulin resistance.
Metabolic flexibility (switching between glucose and fat metabolism).
Potential autophagy (cellular repair processes).
6. What are the risks of prolonged fasting?
Answer:
Insulin resistance (temporary but pronounced after 48+ hours).
Muscle breakdown for gluconeogenesis.
Electrolyte imbalances or refeeding syndrome if food is reintroduced too quickly.
Hormonal disruptions (e.g., cortisol spikes, menstrual irregularities).
7. How can I fast safely without triggering harmful insulin resistance?
Answer:
Start gradually: Begin with 12–16 hour fasts (e.g., 16:8 intermittent fasting).
Stay hydrated: Drink water and electrolyte solutions (no calories).
Prioritize nutrition: Eat fiber-rich, whole foods during eating windows.
Monitor symptoms: Break the fast if dizziness, confusion, or extreme fatigue occurs.
Avoid extremes: Limit prolonged fasting (>72 hours) unless medically supervised.
8. Is fasting safe for everyone?
Answer:
No. Fasting is not recommended for:
Pregnant or breastfeeding women.
Individuals with diabetes, hypoglycemia, or eating disorders.
Those with kidney/liver disease or a history of electrolyte imbalances.
Always consult a healthcare provider before starting any fasting regimen.
9. How does fasting compare to starvation diabetes?
Answer:
Starvation diabetes: A survival mechanism during prolonged calorie deprivation, marked by insulin resistance to spare glucose for the brain.
Voluntary fasting: A controlled practice that temporarily mimics starvation diabetes but is typically reversed with refeeding.
Healthy individuals can use fasting for metabolic benefits, while extreme fasting risks harm.
10. Can fasting "cure" insulin resistance?
Answer:
Short-term fasting may improve insulin sensitivity in healthy or overweight individuals by reducing fat stores and lowering insulin levels.
However, prolonged fasting can temporarily worsen insulin resistance.
Long-term metabolic benefits depend on balanced nutrition and lifestyle habits post-fast.
Key Takeaway
Voluntary fasting can mirror aspects of starvation diabetes, but outcomes depend on duration, health status, and approach.
While short-term fasting offers metabolic benefits, prolonged fasting requires caution and medical guidance.
Always tailor fasting practices to your individual needs and health conditions.