sleep quality : chronic illness and fasting
Explore how chronic illness and fasting affect sleep quality. Learn strategies to improve rest and manage symptoms through mindful fasting practices.
SLEEP
Dr Hassan Al Warraqi
3/3/20257 min read


Optimize Sleep : Chronic Diseases , Medications and fasting
Why Sleep Is Essential for Health
Sleep is a biological powerhouse critical for:
Physical Restoration: Repairs tissues, boosts immunity, and regulates hormones (e.g., growth hormone).
Brain Function: Consolidates memories, enhances learning, and clears metabolic waste via the glymphatic system.
Emotional Balance: Reduces stress, stabilizes mood, and lowers risks of anxiety/depression.
Longevity: Poor sleep is linked to obesity, diabetes, heart disease, and dementia.
Stages of Sleep: What Happens Each Night
Sleep cycles (90–120 minutes) include:
NREM 1 (Light Sleep): Transition phase; easily disrupted.
NREM 2: Heart rate slows; prepares for deep sleep (≈50% of total sleep).
NREM 3 (Deep Sleep): Vital for physical repair; strengthens immunity.
REM Sleep: Dreaming occurs; supports memory and creativity.
Aim for 4–6 cycles nightly (7–9 hours for adults).
Common Sleep Disorders
Insomnia: Difficulty falling/staying asleep (affects 30% of adults).
Sleep Apnea: Breathing pauses during sleep; linked to snoring and fatigue.
Restless Legs Syndrome (RLS): Urge to move legs at rest.
Narcolepsy: Sudden daytime sleep attacks.
Science-Backed Tips for Better Sleep
Fix Your Schedule: Sleep/wake at the same time daily (even weekends).
Optimize Your Environment:
Temperature: 60–67°F (15–19°C).
Light: Use blackout curtains; avoid screens 1–2 hours before bed.
Mind Your Diet:
Avoid caffeine after noon and heavy meals at night.
Try sleep-friendly snacks: Almonds, cherries, or chamomile tea.
Daytime Habits:
Exercise earlier (avoid vigorous workouts close to bedtime).
Get sunlight in the morning to reset your circadian rhythm.
Wind Down: Meditation, reading, or a warm bath signal your body to sleep.
How Chronic Conditions Disrupt Sleep
Diabetes: Nocturia (frequent urination) and nerve pain.
Heart Disease: Shortness of breath when lying down.
Mental Health: Anxiety and depression worsen insomnia.
Medications: Beta-blockers, steroids, and antidepressants often interfere with sleep stages.
Effects of Poor Sleep
Short-Term: Fatigue, poor focus, irritability.
Long-Term: Increased risks of chronic diseases, weakened immunity, and cognitive decline.
SEO Keywords:
Stages of sleep
How to sleep better
Sleep disorders
Sleep hygiene tips
REM vs. deep sleep
Meta Description:
Discover why sleep matters, how it works, and science-backed strategies to improve sleep quality. Learn about sleep stages, disorders, and tips for battling insomnia—optimize your rest today!
SEO-Optimized Content: Chronic Diseases, Medications, Fasting, and Their Impact on Sleep
1. Chronic Diseases and Sleep Disorders
Key Conditions & Their Effects
Diabetes:
Hyperglycemia: Frequent nighttime urination (nocturia) disrupts sleep.
Neuropathy: Limb pain delays sleep onset.
Hypoglycemia: Night sweats and palpitations cause sudden awakenings.
Heart Disease:
Heart Failure: Fluid buildup leads to shortness of breath when lying down (orthopnea).
Arrhythmias: Nighttime heart palpitations increase anxiety.
Respiratory Disorders (Asthma, COPD):
Nighttime coughing and overlapping sleep apnea disrupt deep sleep.
Neurological Disorders (Alzheimer’s, Parkinson’s):
Restless Legs Syndrome (RLS): Tingling sensations prevent relaxation.
REM Sleep Behavior Disorder: Abnormal nighttime behaviors.
2. Medications That Harm Sleep Quality
Common Examples:
Beta-Blockers (e.g., metoprolol): Reduce melatonin → insomnia or nightmares.
Corticosteroids (e.g., prednisone): Increase mental alertness → sleep difficulties.
Antidepressants (e.g., fluoxetine): Trigger night sweats or restlessness.
Opioids: Suppress REM sleep → unrefreshing rest.
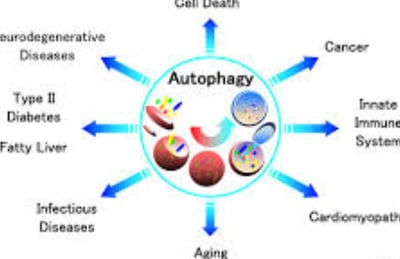
3. Fasting and Sleep: Benefits vs. Risks
Benefits of Fasting:
Circadian Rhythm Alignment: Intermittent fasting (e.g., 16:8) regulates sleep-wake cycles.
Melatonin Boost: Avoiding late-night meals enhances sleep hormone production.
Stable Blood Sugar: Prevents disruptive nighttime spikes/drops.
Risks of Fasting:
Hunger & Stress: Elevated cortisol → difficulty falling asleep.
Dehydration: Muscle cramps from inadequate hydration.
Nutrient Deficiencies: Low magnesium/potassium → insomnia.
4. Tips to Improve Sleep with Chronic Illness , Fasting
For Chronic Disease Patients:
Adjust Medication Timing: Take stimulants (e.g., steroids) in the morning; sedatives at night.
Optimize Sleep Environment: Dark, quiet room (18–20°C / 64–68°F).
Avoid Nighttime Stimulants: Limit caffeine after noon; avoid screens 2 hours before bed.
For Those Fasting:
Time Fasting Wisely: Avoid >16-hour fasts if prone to insomnia; finish meals 3 hours before bed.
Eat Magnesium-Rich Foods: Spinach, nuts, dark chocolate.
5. High-Risk Groups for Sleep Issues
Elderly: Multiple medications + age-related sleep changes.
Diabetes/Heart Patients: Disease-drug interactions worsen sleep.
Mental Health Disorders: Anxiety/depression amplify insomnia.
Key Takeaways
Chronic diseases and medications create a “perfect storm” for sleep disruptions.
Fasting can improve sleep for some but harm others—personalize your approach.
Solutions: Manage diseases effectively, adjust medications, and prioritize sleep hygiene.
SEO Keywords:
Chronic diseases and sleep disorders
Medication side effects on sleep
Intermittent fasting and sleep quality
Insomnia treatment for diabetics
Healthy sleep tips for chronic illness
Meta Description:
Discover how chronic diseases, medications, and fasting impact sleep quality. Learn science-backed tips to improve rest while managing health conditions—optimize your sleep today!
FAQs about sleep
chronic diseases and fasting
How important is sleep for the body and brain?
Sleep is essential for many brain functions, including communication between neurons.
It plays a role in removing toxins that build up in the brain while awake.
Sleep affects almost every tissue and system in the body, including the brain, heart, and lungs, as well as metabolism, immune function, mood, and disease resistance.
Chronic lack of sleep or poor quality sleep increases the risk of health problems such as high blood pressure, cardiovascular disease, diabetes, depression, and obesity.
What are the different stages of sleep, and what happens during each stage?
There are two main types of sleep:
Rapid eye movement (REM)
and non-rapid eye movement (NREM) sleep.
NREM sleep consists of three different stages:
Stage 1 NREM: The transition from wakefulness to sleep. Heart rate, breathing, and eye movement slow down, and muscles relax with occasional twitches. Brain waves begin to slow down.
Stage 2 NREM: Light sleep before entering deep sleep. Heart rate and breathing slow further, and muscles relax further.
Body temperature drops and eye movement stops.
Brain wave activity slows, but is characterized by brief bouts of electrical activity.
Stage 3 NREM: Deep sleep necessary for feeling refreshed in the morning.
Heart rate and breathing slow to their lowest levels.
Muscles are relaxed and you may be difficult to wake. Brain waves slow down.
Rapid eye movement (REM) sleep:
Rapid eye movement occurs about 90 minutes after falling asleep.
Your eyes move rapidly from side to side behind closed eyelids.
Brain wave activity becomes more like what you see when you are awake.
Your breathing becomes faster and irregular, and your heart rate and blood pressure increase to levels close to waking.
Most of your dreams occur during REM sleep.
Your arm and leg muscles become temporarily paralyzed, preventing you from acting out your dreams.
How is sleep regulated in the brain?
Multiple structures within the brain are involved in sleep.
The hypothalamus, located deep within the brain, the brainstem, thalamus, and pineal gland play a role in regulating sleep-wake cycles.
The suprachiasmatic nucleus (SCN) within the hypothalamus controls your circadian rhythm by receiving information about light exposure from the eyes.
The brainstem secretes the chemical GABA to reduce activity and promote sleep, while the pineal gland promotes sleep by producing melatonin.
What is circadian rhythm and how does it affect sleep?
The circadian rhythm is an internal biological process that governs a wide range of functions, from daily changes in alertness to body temperature, metabolism, and hormone release.
This rhythm is influenced by light, as specialized cells in the retina transmit information about light to the brain, which influences the sleep-wake cycle.
The circadian rhythm is based on a 24-hour biological clock.
What is the recommended amount of sleep for different age groups?
Sleep needs vary with age.
Newborns need 14 to 17 hours a day. School-age children and teens need about 9.5 hours of sleep each night. Most adults need 7 to 9 hours of sleep a night.
What factors affect sleep quality?
Factors that affect sleep quality include medical conditions, medications, stress, sleep environment, age, and what you eat and drink. Exposure to light is the biggest influencer.
In addition, consuming caffeine and nicotine late in the day, and drinking alcohol before bed can disrupt sleep.
What are some tips for improving sleep quality?
Establish a sleep schedule – go to bed and wake up at the same time every day.
Exercise for at least 30 minutes most days of the week, but not within a few hours of bedtime.
Avoid caffeine and nicotine late in the day and alcohol before bed.
Relax before bed — try a warm bath, reading, or another relaxing routine.
Create a sleep room — avoid bright lights and loud noises, keep the room temperature comfortable, and don’t watch TV or use a smartphone or computer in your bedroom.
Don’t lie in bed awake.
If you can’t sleep, do something else, such as reading or listening to soothing music, until you feel tired.
What are common sleep disorders, and what tests can be done to diagnose them?
Common sleep disorders include insomnia, sleep apnea, and restless legs syndrome.
Your health care provider can help identify any sleep disorders you have by performing tests such as a polysomnogram or other tests.
These tests can help determine whether you’re reaching and progressing through the different stages of sleep correctly.
The results can be used to develop a treatment plan or determine whether further testing is needed.
What medical conditions and medications can affect sleep?
Many medical conditions and medications can affect sleep, including:
Medical Conditions
Low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia), cardiovascular disease, respiratory disease, neurological disorders (such as Parkinson's and Alzheimer's disease), and mental health disorders (such as depression and anxiety).
Medications
Beta-blockers, corticosteroids, antidepressants, stimulants, chemotherapy agents, diuretics, opioid painkillers, antidepressants,
Antihistamines.
How does fasting affect sleep and are there precautions to take?
Voluntary fasting (such as intermittent fasting, time-restricted eating, or extended fasting) can affect sleep in both positive and negative ways, depending on factors such as the duration and timing of fasting and individual physiology.
Positive effects
Improves circadian rhythm alignment, increases melatonin production, and reduces blood sugar fluctuations.
Negative effects
Hunger and discomfort, low blood sugar, increased cortisol and alertness, and dehydration.
Precautions
Monitor your body, adjust your eating window, and consult a healthcare professional if fasting causes insomnia or fatigue. People with a history of eating disorders, adrenal fatigue, chronic stress, or individuals taking medications that require eating should be cautious.