Rabies : Always deadly: No cure
Learn about rabies, a viral disease affecting the central nervous system transmitted through the bite of infected animals. Discover the importance of prompt treatment, prevention methods, vaccines,...
NERVOUS SYSTEM
Dr Hassan Al Warraqi
10/3/2023


Understanding Rabies: Symptoms, Treatment, and Prevention
Rabies is a viral disease that can be fatal if not treated promptly.
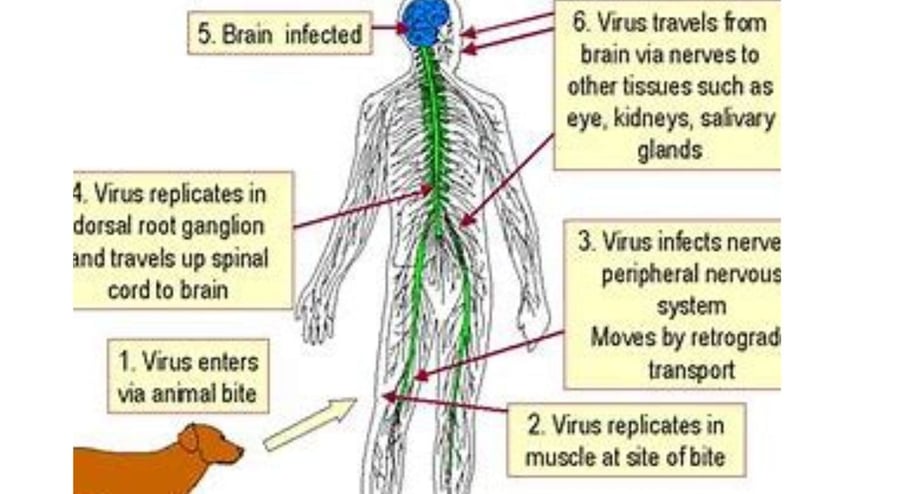
It is caused by a virus that attacks the central nervous system.
Rabies can be transmitted through the bite of an infected animal, such as a dog, bat, or raccoon.
The symptoms of rabies
can vary depending on the severity of the infection.
In the early stages, symptoms may include fever, headache, fatigue, and muscle aches. As the infection progresses, symptoms may become more severe and include difficulty swallowing, excessive salivation, and hydrophobia (fear of water). In the final stages of the infection, paralysis and coma can occur.
There is no cure for rabies once symptoms develop.
However, if treatment is started early, it can be possible to prevent the disease from progressing.
If you are bitten by an animal, it is important to follow these steps:
Wash the wound immediately with soap and water.
Seek medical attention immediately.
If you are not sure if the animal is infected with rabies, the doctor may recommend starting rabies treatment.
don't close the open wounds
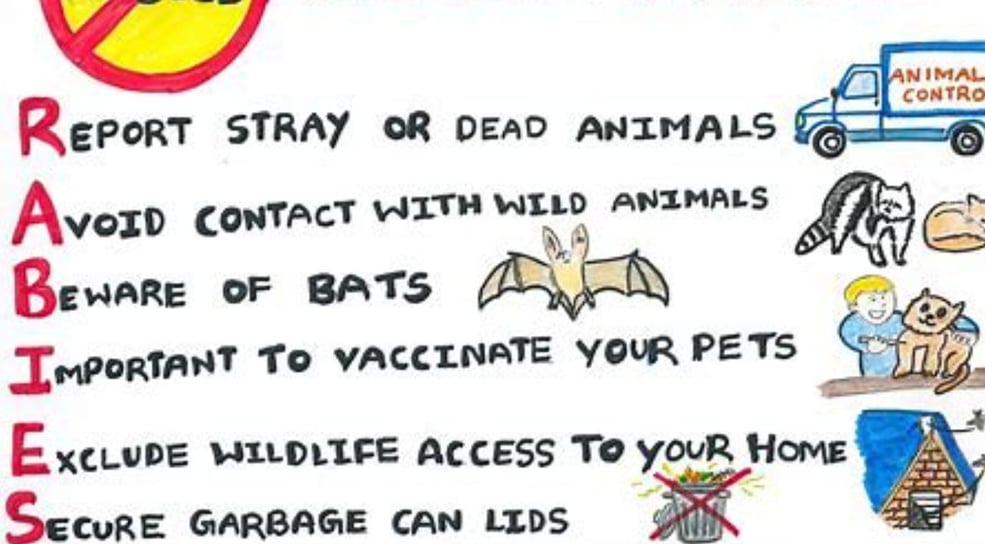
The best way to prevent rabies is to avoid contact with wild animals. This includes:
Do not feed or touch wild animals.
Keep your distance from wild animals, especially if they are acting strangely.
Supervise children closely around wild animals.
If you find a wild animal that is injured or orphaned, keep away .
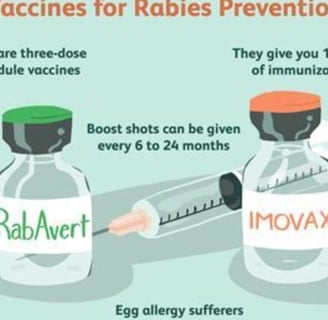
These vaccines are recommended for people who are at high risk of exposure to rabies, such as:
Veterinarians
Animal handlers
People who work in areas where rabies is common
People who travel to countries where rabies is common
Here are some additional tips for preventing rabies:
Keep your pets vaccinated against rabies.
Have your pets spayed or neutered.
Do not allow your pets to roam free outside.
Supervise your pets closely when they are around other animals.
By following these tips, you can help to protect yourself and your loved ones from rabies.
Rabies prevention
There are a number of things that can be done to prevent rabies, including:
Vaccinating pets: This is the most important way to prevent rabies in humans. Pets should be vaccinated against rabies according to the recommendations of their veterinarian.
Keeping pets under control: Pets should not be allowed to roam free outside, as this increases the risk of them coming into contact with wild animals that may be infected with rabies.
Supervising children around animals: Children should be supervised closely around all animals, both domestic and wild. This will help to prevent them from being bitten or scratched.
Reporting stray animals: If you see a stray animal, contact your local animal control agency. Stray animals are more likely to be infected with rabies than domesticated animals.
Rabies treatment
If you are bitten by an animal and you are not sure if it is infected with rabies, it is important to seek medical attention immediately.
Treatment for rabies infection typically involves a series of injections of rabies immunoglobulin and rabies vaccine.
Rabies immunoglobulin: This is given to provide immediate protection against the virus. It is made from the blood serum of people who have been vaccinated against rabies.
Rabies vaccine: This is given to help the body develop long-term immunity to the virus. It is made from a weakened form of the rabies virus.
The number of injections and the length of time between injections will depend on the severity of the exposure and the patient's age.
If you are bitten by an animal, it is important to follow these steps:
Wash the wound immediately with soap and water.
Seek medical attention immediately.
If you are not sure if the animal is infected with rabies, the doctor may recommend starting rabies treatment.
Rabies is a serious disease, but it is preventable. By following these steps, you can help to protect yourself and your loved ones from rabies.
Additional information about rabies treatment
is most effective if started within 24 hours of exposure to the virus. However, treatment can still be effective if started later, up to 72 hours after exposure.
several health authorities said that latent rabies appear year after exposure .
If you are receiving rabies treatment, it is important to complete the full course of injections, even if you start to feel better.
This will help to ensure that you are fully protected against the virus.
There is no cure for rabies once symptoms develop.
However, early treatment can help to prevent the disease from progressing.
no harm to apply fasting or intermittent fasting.
key words
rabies,central nervous system,bite of infected animals'treatment,prevention,vaccine immunoglobulin,stray animals',symptoms ,started within 24 hours of exposure to the virus,fasting or ,intermittent fasting,
,
Rabies
Rabies is a deadly viral disease that attacks the central nervous system of mammals, including humans.
It is primarily transmitted through the saliva of infected animals, typically via bites, scratches, or contact with open wounds and mucous membranes.
One of the oldest known diseases, rabies has no effective cure once symptoms appear, but it can be prevented through pre- and post-exposure vaccination.
Nature and Cause of the Disease
Rabies is caused by a virus from the Rhabdoviridae family, specifically the Lyssa virus. The virus targets the central nervous system, causing severe brain inflammation.
"Rabies is an infectious viral disease transmitted from infected animals to humans and pets through bites or scratches, leading to brain inflammation and potentially death if untreated."
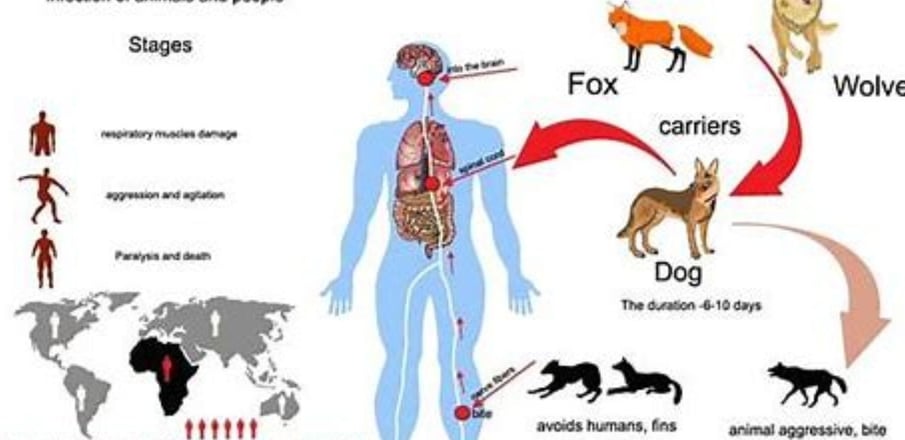
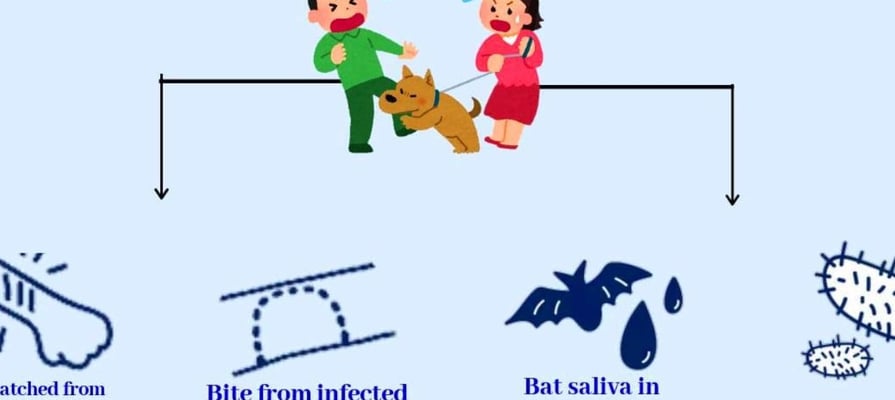
Transmission Methods
The virus spreads through the saliva of infected animals, with dogs responsible for 99% of human rabies cases globally. Transmission occurs via:
Bites: The most common route.
Scratches or licking wounds: The virus can enter through damaged skin or mucous membranes (mouth, nose).
Other animals: Including cats, bats, foxes, wolves, and mongooses. Human-to-human transmission is extremely rare.
"The virus cannot penetrate intact skin but can enter through wounds or mucous membranes."
"Dogs cause 96% of rabies cases in Southeast Asia."
Incubation Period
The incubation period typically ranges from 2 to 10 weeks but can vary from 4 days to several years, depending on:
The location and severity of the wound.
The amount of virus transmitted. In over 90% of cases, the incubation period is less than a year.
"The incubation period is usually 20-90 days, rarely extending to years."
"It depends on the wound’s location and viral load."
Symptoms
Initial symptoms resemble the flu, including:
Fever, headache, fatigue, nausea, sore throat, dry cough.
These progress to:
Agitation, insomnia, confusion, abnormal behavior.
Hallucinations, hydrophobia (due to painful throat spasms).
Partial paralysis, coma, and death within days of clinical symptoms.
"Hydrophobia prevents swallowing due to throat spasms."
"Symptoms evolve into delirium and paralysis."
Diagnosis
No effective diagnostic tools exist before symptoms appear.
Clinical diagnosis relies on linking symptoms to exposure to an infected animal.
Confirmation occurs post-mortem by detecting the virus or its antigens in tissues.
"Diagnosis is challenging without distinctive symptoms like hydrophobia."
Treatment
Once symptoms appear, rabies is almost always fatal, with no effective treatment.
Supportive care: May prolong life but rarely saves the patient.
Milwaukee Protocol: A rare treatment attempt with limited success.
"Death occurs within 2-10 days of symptoms."
"No specific treatment exists for classic rabies."
Post-Exposure Prophylaxis (PEP)
Post-exposure prophylaxis is critical to prevent rabies progression and includes:
Wound cleaning: Wash with soap and water for 10-15 minutes.
Disinfection: Use an antiseptic like alcohol or iodine.
Vaccination: Administer rabies vaccine and, if needed, human rabies immunoglobulin (HRIG) based on exposure severity.
"Wound cleaning is the most effective first aid."
"PEP is required for bleeding wounds or mucous membrane exposure to saliva."
Pre-Exposure Prophylaxis (PrEP)
Rabies vaccines are recommended for high-risk individuals, such as:
Veterinary lab workers.
Those handling wild animals (bats, foxes).
Travelers to endemic areas (Asia, Africa).
Children in high-risk regions.
"Vaccines are essential for animal handlers and travelers."
Animal Control
Preventive measures include:
Pet vaccination: Regular shots for dogs and cats.
Stray animal control: Reducing exposure to infected animals.
Monitoring biting animals: Observing for 10 days to check for rabies signs.
"Pet vaccination is a key preventive step."
"Supervise pets to avoid contact with wildlife."
Geographic Distribution
Rabies is widespread globally but is more common in:
Asia and Africa: Dogs are the primary vector.
The Americas: Bats and raccoons alongside dogs.
Western Europe and Oceania: Mostly limited to bats.
"Dogs cause 99% of human cases globally."
"Bats account for 98% of U.S. cases."
Historical Significance
Rabies has been feared throughout history due to its violent symptoms.
Louis Pasteur’s 1885 vaccine marked a turning point in its control.
"Rabies was known since 2000 BCE for its aggressive nature."
"Before Pasteur’s vaccine, all cases were fatal."
Challenges in Developing Countries
Inadequate animal vaccination programs.
Poor control of stray animals.
Limited access to post-exposure treatment.
"Stray dogs increase risks in developing nations."
Keys to Success
Education and awareness: Spreading prevention knowledge.
Vaccination: For humans and animals.
Surveillance: Tracking cases and infected animals.
Collaboration: Between health and veterinary sectors.
"Education and vaccination are key to control."
Conclusion
Rabies is a preventable yet deadly viral disease. Rapid intervention, vaccination, and awareness are critical to curbing its spread.
Eliminating rabies requires ongoing collaboration between health, veterinary, and community sectors for effective control.
SEO Keywords
Rabies, rabies virus, rabies vaccine, rabies symptoms, rabies prevention, rabies treatment, rabies transmission, dogs and rabies, hydrophobia, rabies shot, Milwaukee Protocol.
Frequently Asked Questions About Rabies FAQS
1. What is rabies and how is it transmitted to humans?
Rabies is a deadly viral disease that affects the central nervous system of mammals, including humans. It is primarily transmitted through the saliva of infected animals, typically via:
Bites: The most common method.
Scratches or licking wounds: The virus can enter through broken skin or mucous membranes (mouth, nose).
Carrier animals: Dogs cause 99% of human rabies cases globally, especially in Asia and Africa. Other animals like bats, foxes, raccoons, cats, and wolves can also transmit it.
Human-to-human transmission is extremely rare, occurring only in exceptional cases like organ or cornea transplants from an infected person.
"The virus spreads through infected saliva and cannot penetrate intact skin."
"Dogs are responsible for most rabies cases in Asia and Africa."
Keywords: Rabies, rabies virus, rabies transmission, dogs and rabies.
2. What are the symptoms of rabies in humans?
Rabies symptoms begin with flu-like signs, including:
Fever, headache, fatigue.
Nausea, vomiting, sore throat, dry cough.
These progress to a severe neurological phase, including:
Hyperactivity: Agitation, insomnia, confusion, abnormal behavior.
Hydrophobia: Difficulty swallowing due to painful throat spasms.
Aerophobia: Extreme sensitivity to air currents.
Muscle spasms, excessive salivation, sweating, hallucinations.
In the final stage, patients develop paralysis, followed by coma and death, often due to respiratory or cardiac failure.
"Hydrophobia is a hallmark symptom of rabies."
"The disease leads to death within days of neurological symptoms."
Keywords: Rabies symptoms, hydrophobia, rabies in humans, signs of rabies.
3. What should I do immediately after an animal bite?
If bitten or scratched by an animal, take these steps immediately:
Wash the wound: Clean the area with soap and water for 10-15 minutes. If soap is unavailable, use water alone.
Disinfect the wound: Apply a 70% alcohol solution or povidone-iodine if possible.
Seek medical care: Visit a healthcare facility as soon as possible for risk assessment and potential treatment.
Avoid harmful actions: Do not apply irritants (e.g., spices) to the wound or cover it with a bandage before medical evaluation.
"Wound cleaning is the most critical first step."
"Early treatment can be lifesaving."
Keywords: Animal bite, rabies first aid, wound cleaning, rabies prevention.
4. When is rabies vaccination necessary after a bite?
Post-exposure prophylaxis (PEP) is necessary in the following cases:
Bleeding bite or scratch: From an animal confirmed or suspected to have rabies (dogs, cats, bats, foxes).
Saliva contact: If an animal’s saliva reaches open wounds or mucous membranes.
Animal behavior: If the animal acts abnormally, disappears, is killed, or tests positive for rabies.
Even vaccinated animals: Treatment may be needed if the animal’s vaccination status is uncertain.
PEP must begin promptly to be effective.
"PEP is essential for suspected rabies exposure."
"Delay can reduce survival chances."
Keywords: Rabies vaccine, post-exposure treatment, rabies PEP, rabies shot.
5. Is there a treatment for rabies after symptoms appear?
Unfortunately, rabies is nearly 100% fatal once neurological symptoms appear, with no effective treatment at this stage.
Rare survival cases (e.g., using the Milwaukee Protocol) involved patients who had prior vaccination or exceptional intensive care.
The primary goal is prevention through:
Rapid intervention after exposure.
Administering vaccines and human rabies immunoglobulin (HRIG) before symptoms develop.
"No specific treatment exists after symptoms."
"Prevention is the only solution."
Keywords: Rabies treatment, rabies after symptoms, Milwaukee Protocol.
6. What are the most important ways to prevent rabies?
Rabies prevention relies on multiple strategies:
Pet vaccination: Regularly vaccinate dogs, cats, and other pets, keeping records.
Pet supervision: Prevent pets from contacting wild animals.
Stray animal control: Report stray dogs or cats to local authorities.
Avoid wild animals: Especially bats, foxes, and raccoons.
Pre-exposure prophylaxis (PrEP): For high-risk groups like veterinarians, animal handlers, or travelers to endemic areas.
Post-exposure actions: Immediately wash wounds and seek PEP if needed.
"Pet vaccination reduces disease spread."
"Avoiding bats protects against infection."
Keywords: Rabies prevention, pet vaccination, rabies control, rabies precautions.
7. What is the role of vaccination in controlling rabies?
Vaccination is critical for rabies prevention and control:
Animal vaccination: Reduces infection in dogs and cats, limiting human transmission.
Human pre-exposure vaccination (PrEP): Protects high-risk individuals like veterinary workers.
Post-exposure vaccination (PEP): Highly effective if started early, preventing disease progression.
Comprehensive animal vaccination programs, combined with accessible human vaccines and immunoglobulin, have significantly reduced rabies cases in many countries.
"Widespread vaccination has eliminated rabies in some regions."
"Human vaccines are effective if given early."
Keywords: Rabies vaccination, rabies shot, rabies control.
8. What are the recent advancements in rabies vaccines and treatments?
Rabies vaccines have seen significant progress:
Tissue culture vaccines: Safe, highly effective, and provide long-lasting immunity.
Freeze-dried vaccines: Extended shelf life, available in single-dose vials.
Intradermal vaccination: A cost-effective, safe method endorsed by the World Health Organization.
In treatment:
Monoclonal antibodies: Being developed to supplement human rabies immunoglobulin (HRIG) supplies.
Milwaukee Protocol: Involves induced coma and intensive care but has low success rates and requires further research.
Ongoing research aims to improve treatments and ensure vaccine availability in developing regions.
"Modern vaccines are safer and more effective."
"The Milwaukee Protocol remains experimental."
Keywords: Rabies vaccine advancements, rabies treatment, Milwaukee Protocol, rabies antibodies.
Conclusion
Rabies is a fatal but preventable disease. Vaccination, prompt wound care, and awareness are key to eliminating its threat.
Advances in vaccines and global control programs bring us closer to eradicating rabies.
Additional Keywords: Rabies virus, rabies cure, rabies signs, rabies animals, preventive vaccination.