Multidisciplinary Treatment : Flesh-Eating disease
Discover effective novel treatments for necrotizing fasciitis, including fasting strategies and multidisciplinary care. Learn how early intervention can prevent organ failure and improve outcomes i...
DIABETES
Dr Hassan Alwarraqi
10/14/202414 min read


Multidisciplinary Treatment : Flesh-Eating disease
its a trouble of diabetes mellitus and out of control blood sugar
Necrotizing fasciitis (NF) and Fournier's gangrene (FG) are two uncommon but life-threatening infections of the soft tissues that require immediate clinical interest
at the same time as NF affects various components of the body, FG mainly objectives the perineal location,
inclusive of the scrotum, penis, and perineum.
both situations contain the fast destruction of gentle tissues and require competitive treatment, often such as surgical procedure and antibiotics.
Necrotizing Fasciitis: The “Flesh-eating” contamination
Necrotizing fasciitis, often known as the flesh-eating disease, is a severe bacterial infection that reasons the dying (necrosis) of the soft tissues,
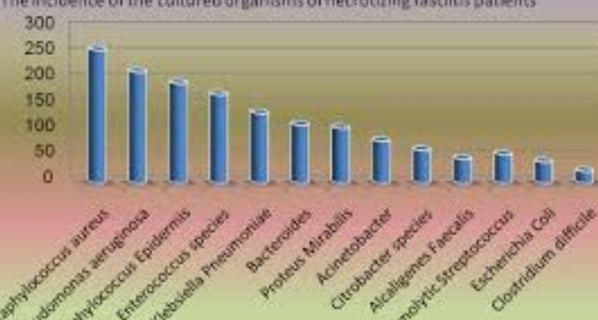
which include fats, muscle, and fascia. The maximum not unusual motive of NF is bacterial infection with the aid of Streptococcus pyogenes, frequently called institution A strep.
but, other micro organism like Clostridium perfringens, Staphylococcus aureus, and Escherichia coli also can contribute to the infection.
The infection spreads rapidly, often within hours, inflicting systemic signs and symptoms including fever, extreme pain, and swelling inside the affected area. If left untreated, necrotizing fasciitis can bring about sepsis, organ failure, and dying.
The differential diagnoses for necrotizing fasciitis
encompass several other conditions, including nonnecrotizing fasciitis, cellulitis, dermatomyositis, and various forms of vasculitis such as lupus myofasciitis and Churg-Strauss vasculitis.
Additionally, graft-versus-host disease (GVHD), diabetic myonecrosis, and compartment syndrome .
Fournier's Gangrene: a selected sort of Necrotizing Fasciitis
Fournier's gangrene is a type of necrotizing fasciitis that affects the genital area, particularly the scrotum, penis, and perineum.
though it may affect both women and men, it's considerably more not unusual in men.
The condition frequently starts off evolving with trauma, surgical wounds, or infections within the genital region and unexpectedly progresses to tissue necrosis.
incision into the deep fascia, probing with the index finger may be in the the extremities (arms, hands, feet and legs .
the initial treatment for necrotizing fasciitis &Fournier's Gangrene
wide, extensive debridement of all tissues . Wide debridement of all necrotic and poorly perfused tissues is associated with more rapid clinical improvement .
The hallmark symptoms of Fournier's gangrene encompass:
- intense pain and swelling in the genital or perineal place.
- Fever, chills, and trendy malaise.
- Tissue discoloration and foul-smelling drainage due to the dying of tissues.
- Crepitus (a crackling sensation underneath the skin) due to gasoline-producing bacteria.
triad of necrotizing fasciitis Fournier's gangrene
progressive erythema, severe dermatological edema and severe pain disproportionate to the physical findings
this cinsider a surgical emergency.
causes of Fournier’s Gangrene and Necrotizing Fasciitis
Fournier’s gangrene and other types of necrotizing fasciitis are resulting from bacterial infections, with polymicrobial (multiple micro organism) involvement in many instances.
some of the maximum commonplace bacteria located in Fournier’s gangrene include:
- Escherichia coli (E. coli)
- Klebsiella species
- Bacteroides species
- Clostridium species (accountable for gas gangrene)
certain danger elements make people more prone to developing these infections:
- Immunocompromised states, together with diabetes or HIV
- current surgical operation or trauma in the affected location
- continual alcohol abuse
- poor hygiene or terrible circulation within the genital region
Fournier's Gangrene vs. Necrotizing Fasciitis
whilst Fournier's gangrene is a specific kind of necrotizing fasciitis, there are a few differences between the 2:
- region: Fournier's gangrene impacts the genital and perineal regions,
while necrotizing fasciitis can arise everywhere in the frame.
- Microbial reasons: Fournier's gangrene regularly entails polymicrobial infections,
while necrotizing fasciitis can be resulting from a single organism, consisting of Streptococcus or Staphylococcus species.
gender : Fournier's gangrene is extra not unusual in men, especially people with risk factors like diabetes,
even as necrotizing fasciitis can arise in each sexes.
Other people who are at greater risk for necrotizing fasciitis include those who:
have chronic heart or lung disease
use steroids
have skin lesions
abuse alcohol or inject drugs
threat elements for necrotizing fasciitis
you can increase necrotizing fasciitis even in case you’re perfectly healthy, however this is rare.
folks that have already got health problems that weaken the immune machine, consisting of most cancers or diabetes, are at extra riskTrusted source of growing infections caused by A Streptococcus.
the types of necrotising fasciitis
Type I (70–80% cases) Polymicrobial, synergistic, often bowel flora-derived
Type II (20–30% cases) Often monomicrobial, skin- or throat-derived
Type III Gram-negative, often marine-related organisms
Type IV (fungal) Usually trauma associated, immunocompetent patients
prognosis and remedy of Fournier’s Gangrene modele remedy
analysis of Fournier’s gangrene is crucial for survival. excisional deep skin biopsy is helpeful
medical doctors depend on a combination of medical examination, laboratory checks, and imaging studies like CT scans to verify the diagnosis.
signs of soft tissue gas or fluid collections within the genital region on a CT experiment can imply Fournier’s gangrene.
modele remedy:
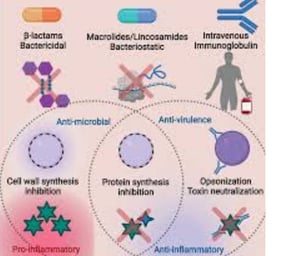
specific treatment Protocols for Necrotizing Fasciitis (NF) and Fournier’s Gangrene (FG)
- Surgical debridement : wide and deep elimination of necrotic (useless) tissue is vital to stop the spread of contamination.
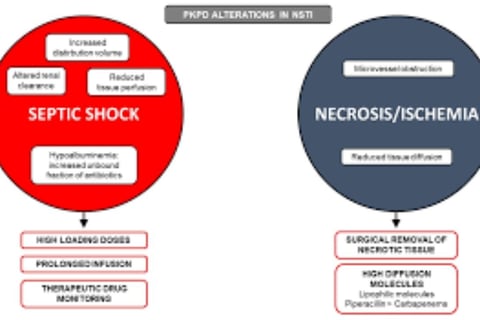
-wide-spectrum antibiotics : Early antibiotic remedy is important to cowl each cardio and anaerobic bacteria.
not unusual antibiotics encompass
piperacillin-tazobactam, clindamycin, and vancomycin.
Repeat Debridement: Serial surgical procedures are commonly required each 24-48 hours until no in addition necrotic tissue is identified.
2nd look surgical procedures are crucial for assessing ongoing tissue viability.
Amputation or Tissue Reconstruction: In severe cases, amputation or plastic reconstructive surgical operation may be important for limb salvage or to close big defects after debridement.
For Fournier's Gangrene (FG):
Debridement ought to encompass the perineum, genitalia, and every now and then increase into the belly wall.
Surgical reconstruction may additionally comply with, once the infection is managed, to repair the perineal vicinity.
along with gram-wonderful, gram-bad, and anaerobic micro organism.
Empirical Antibiotic routine:
- Polymicrobial insurance is critical, and the routine regularly consists of:
1. Carbapenem (e.g., imipenem or meropenem) or a beta-lactam/beta-lactamase inhibitor (e.g., piperacillin-tazobactam)
2. Clindamycin: crucial for its capability to inhibit bacterial toxin production, specifically in group A Streptococcal infections.
3. Vancomycin or Linezolid: For MRSA (Methicillin-resistant Staphylococcus aureus) coverage.
4. Metronidazole or coverage for anaerobes may also be blanketed if extensive-spectrum activity in opposition to anaerobes isn't ensured by means of the number one antibiotic (if the usage of piperacillin-tazobactam or a carbapenem, anaerobe coverage is commonly sufficient).
Pathogen-particular modifications:
as soon as subculture and sensitivity consequences are available, the antibiotic regimen may be narrowed based totally on the particular organisms involved:
- If Streptococcus pyogenes (organization A Streptococcus) is diagnosed, retain with Penicillin G plus Clindamycin.
- For MRSA, Vancomycin, Linezolid, or Daptomycin should be maintained.
- aerobic gram-negative infections, like Escherichia coli or Klebsiella, might also require changes to include 0.33-era cephalosporins (e.g., ceftriaxone) or fluoroquinolones.
period of remedy:
- IV antibiotics are continued for 10-14 days, often longer relying on medical response and the number of surgical procedures required.
- Transition to oral antibiotics can be taken into consideration as soon as the infection is properly-managed and no in addition debridements are vital.
remedy usually lasts several weeks, relying at the extent of infection.
Supportive care : sufferers frequently require intensive care, together with fluids, blood pressure help, and possible pores and skin grafts or reconstructive surgical procedure after the infection is managed.
Supportive Care
patients with necrotizing fasciitis and Fournier's gangrene often require extensive care due to sepsis, organ dysfunction, and the want for frequent surgeries.
Fluid Resuscitation
- aggressive intravenous fluids to maintain hemodynamic stability, in particular if the affected person is in septic surprise.
- Vasopressors (e.g., norepinephrine ) may be required in sufferers with refractory hypotension in spite of good enough fluid resuscitation.
monitoring and management of Organ Failure:
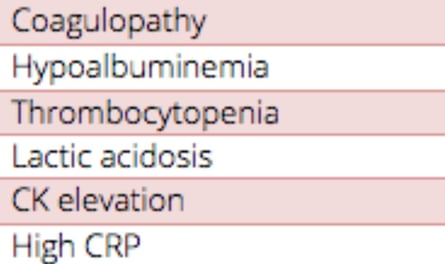
Sepsis protocols have to be accompanied, together with tracking for acute kidney damage , respiratory failure , and coagulopathy (DIC - disseminated intravascular coagulation).
Mechanical ventilation or renal replacement therapy (dialysis) can be required for patients with multi-organ failure.
dietary aid
- Early enteral feeding is suggested while possible to save you malnutrition, sell recuperation, and assist immune feature.
Adjunctive remedies
though much less hooked up, sure adjunctive treatments can be beneficial in a few instances of necrotizing fasciitis and Fournier's gangrene:
Intravenous Immunoglobulin (IVIG):
IVIG may be considered, mainly in toxin-mediated infections which includes group A Streptococcal necrotizing fasciitis. The motive is to neutralize bacterial pollution and modulate the immune reaction.
Dose: usually, 1-2 grams/kg administered as a single or divided dose.
Hyperbaric Oxygen remedy (HBOT):
- some protocols include HBOT as an adjunctive treatment to increase oxygen transport to tissues, enhance the killing of anaerobic bacteria, and sell wound recuperation.
- HBOT is commonly used submit-debridement in specialised centers, although its normal gain remains debated.
lengthy-time period Care and Rehabilitation
once the contamination is managed and the affected person is stabilized, a focal point on wound control and rehabilitation is critical:
Wound Care: negative stress wound therapy (vacuum-assisted closure or VAC) can be used to help with wound restoration and minimize fluid buildup.
pores and skin Grafts and Reconstruction: big tissue defects might also require pores and skin grafts or flap reconstruction by means of plastic surgeons.
Rehabilitation: physical therapy is often vital, in particular for sufferers who have undergone amputations or good sized surgical procedures.
in short
coping with necrotizing fasciitis and Fournier's gangrene calls for a
multidisciplinary teams method related to surgeons, infectious disorder specialists, intensivists, and wound care professionals. Early analysis,
set off surgical debridement, and extensive-spectrum antibiotics are the cornerstones of remedy, with
repeated exams to guide further management. With timely and suitable interventions, the mortality fee, though high, can be decreased notably.
Fasting
isn't always a well known or endorsed treatment for Fournier's gangrene or necrotizing fasciitis.
both of those conditions are excessive, rapidly progressing infections that require immediate medical interventions,
which includes surgery and antibiotics, to control the infection
but, fasting or particular nutritional practices may not directly impact the overall health of a patient, especially if they're dealing with situations like diabetes, that is a recognized risk element for each Fournier’s gangrene and necrotizing fasciitis.
Diabetes and Fasting : some people with diabetes can also use intermittent fasting to assist manage blood sugar levels.
considering that uncontrolled diabetes can predispose people to infections like Fournier's gangrene, better blood sugar control may want to theoretically decrease the hazard of such infections.
That said, fasting have to be done below clinical supervision, particularly for the duration of recuperation, as bad nutrition or hypoglycemia ought to negatively impact healing.
Fasting during vital contamination : inside the context of treating Fournier's gangrene or necrotizing fasciitis, fasting could be dangerous rather than helpful.
these infections result in fast tissue destruction, infection, and systemic contamination, that can require accelerated dietary guide to promote healing and restoration.
Fasting may want to deprive the frame of the nutrients and power it wishes to combat off infection and get over surgical operation.
Surgical and Operative Care : put up-surgical sufferers typically want balanced nutrition to help immune feature, wound recovery, and recovery.
Fasting at some point of this era should gradual restoration or get worse consequences, particularly in sufferers who are already susceptible.
In precis, at the same time as fasting may also have health blessings in positive contexts, there's no evidence that it performs a beneficial role in the remedy of Fournier's gangrene or necrotizing fasciitis.
In reality, in severely ill patients or the ones getting better from most important surgery, adequate vitamins is essential for restoration and restoration.
It’s critical for patients with these infections to observe their healthcare group’s steering intently, which normally includes aggressive scientific and surgical interventions in preference to nutritional adjustments like fasting.
fasting specially islamic one is critical if implemented throughout
fasting early in the disease
- severe ache and swelling within the genital or perineal location.
- Fever, chills, and general malaise.
- Tissue discoloration and foul-smelling drainage due to the loss of life of tissues.
- Crepitus (a crackling sensation beneath the skin) due to gas-generating bacteria.
fasting for control & prevention of Organ Failure
helpful in Sepsis , acute kidney injury , breathing failure and coagulopathy (DIC - disseminated intravascular coagulation.
fasting prevent and treat type 2 diabetes. Benefits include improved insulin sensitivity, lowered blood pressure, reduced body fat and risk of CVD.
Necrotizing fasciitis, Flesh-Eating disease ,Fournier’s gangrene , novel treatment , fasting , islamic , early in the disease , organ failure , fasting control diabetes ,multidisciplinary teams ,period of remedy IV antibiotics for 10-14 days,Supportive Care,control blood sugar ,fast destruction of gentle tissues , fats, muscle, and fascia ,
https://emedicine.medscape.com/article/784690-overview
https://www.healthline.com/health/necrotizing-soft-tissue-infection
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2762295/
https://www.sciencedirect.com/science/article/pii/S0012369215463068
https://www.cdc.gov/group-a-strep/about/necrotizing-fasciitis.html
Necrotizing Fasciitis (NF) -"Flesh-Eating Disease"
What is Necrotizing Fasciitis?
Necrotizing Fasciitis is a rare but severe bacterial infection, often referred to as "flesh-eating disease." It leads to the rapid destruction of soft tissues, including the skin, muscles, and fat.
Understanding this condition, its causes, symptoms, and treatment is critical to preventing serious complications that can lead to death.
Definition: It is a bacterial infection that affects the soft tissues under the skin, specifically the fascia (the connective tissue surrounding muscles).
Rapid Destruction: It is characterized by the rapid breakdown of soft tissues, not the direct "eating" of tissue as the term "flesh-eating disease" suggests.
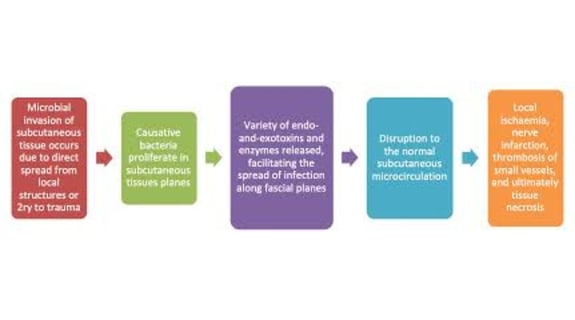
Mechanism: The bacteria release toxins that damage tissues, along with the immune system's response, which exacerbates the condition.
Types of Necrotizing Fasciitis:
Type I (Polymicrobial):
Most common (70-80% of cases), caused by a mix of bacteria, often from intestinal bacteria.
Includes Staphylococcus aureus, Streptococcus pyogenes, and various Clostridium species.
Type II (Mono-microbial):
Accounts for 20-30% of cases, often caused by Streptococcus pyogenes or methicillin-resistant Staphylococcus aureus (MRSA).
Type III:
Caused by Vibrio vulnificus, found in saltwater environments.
Type IV (Fungal):
Rare, caused by fungi like Candida albicans.
Often linked with trauma or immunocompromised patients.
Causes and Risk Factors:
Wounds: Infection often begins through cuts, scrapes, or other skin injuries.
Weakened Immune System: Those with conditions like diabetes, cancer, or HIV are at higher risk.
Other Risk Factors: Alcohol use, intravenous drug use, obesity, and vascular diseases.
Symptoms:
Severe Pain: Often disproportionate to the size of the wound or injury.
Redness and Swelling: The area may initially appear as a simple skin infection but worsens rapidly.
Skin Discoloration: The skin may turn purple or black, with blisters forming.
Systemic Symptoms: Fever, chills, hypotension, and in severe cases, loss of consciousness.
Diagnosis:
Clinical Examination: Based on symptoms and physical examination.
Surgical Examination: A key diagnostic test involves "finger examination," where tissues separate easily along the fascia.
Laboratory Tests: Blood tests like CBC and CRP levels.
Imaging:
CT scans to identify fascial thickening, edema, and gas buildup.
MRI for detecting deeper fluid accumulations.
Ultrasound (POCUS) to assess subcutaneous tissue changes.
Treatment:
Surgery: Essential for removing dead tissue (debridement) and preventing the spread of infection, often requiring multiple procedures.
Antibiotics: Broad-spectrum IV antibiotics to treat a variety of bacteria.
Additional Treatments:
Hyperbaric Oxygen Therapy (HBO) for aiding wound healing and killing anaerobic bacteria.
Intravenous Immunoglobulin (IVIG) for infections involving toxins, like in necrotizing fasciitis caused by Streptococcus.
Wound care, including Negative Pressure Wound Therapy (VAC).
Fournier's Gangrene:
A form of necrotizing fasciitis affecting the genital area.
Symptoms: Severe pain, swelling, tissue discoloration, foul-smelling discharge.
Treatment: Similar to NF, including surgery and antibiotics.
Complications:
Sepsis
Shock
Organ failure
Amputation
Large, permanent scars
Death
Prevention:
Proper wound care and hygiene.
Covering open wounds.
Managing chronic conditions like diabetes.
Psychological Aspects:
Patients may face depression or PTSD following the experience.
History:
First described by Hippocrates in the 5th century BCE.
Famous Cases: Several high-profile cases have been reported, involving public figures contracting necrotizing fasciitis.
Fasting:
Early fasting may help control organ failure and prevent diabetes, particularly in the early stages of the disease.
Myths:
Contrary to the name "flesh-eating disease," the bacteria do not directly eat flesh. They release toxins that destroy tissues.
Conclusion:
Necrotizing fasciitis is a life-threatening condition requiring urgent medical intervention.
Understanding the disease's causes, symptoms, and treatment options is critical for reducing severe complications and saving lives. Awareness of proper wound care, good hygiene, and managing chronic conditions are essential preventive steps.
Frequently Asked Questions (FAQs) about Necrotizing Fasciitis (Flesh-Eating Disease)
What is Necrotizing Fasciitis (Flesh-Eating Disease)?
Necrotizing Fasciitis is a rare but serious bacterial infection that affects the soft tissues under the skin, including fat, muscles, and fascia (the connective tissue surrounding muscles).
It is characterized by rapid tissue destruction and is often referred to as "flesh-eating disease" because of its fast spread and tissue death.
However, the bacteria do not literally "eat" the tissue; instead, they release toxins that cause the tissue to break down.
What are the causes of Necrotizing Fasciitis?
The infection typically occurs when different types of bacteria enter the body through a wound, scrape, or cut in the skin.
Common bacteria include:
Group A Streptococcus (Streptococcus pyogenes), which also causes strep throat.
Staphylococcus aureus.
Anaerobic bacteria like Clostridium, and other bacteria such as Escherichia coli.
Certain medical conditions increase the risk, including diabetes, a weakened immune system, alcohol or drug injection use, recent surgery, or trauma.
What are the symptoms of Necrotizing Fasciitis? How can I recognize it early?
Early symptoms include severe pain in the affected area, which is often disproportionate to the size of the injury or wound.
This is followed by swelling and redness, and the skin may turn darker with the development of ulcers or blisters filled with fluid. The patient may also experience fever and chills. In advanced cases, low blood pressure and loss of consciousness may occur. It is important to seek emergency care immediately if these symptoms appear, especially if the pain increases rapidly.
Is Necrotizing Fasciitis contagious?
Necrotizing Fasciitis is not highly contagious, but it can spread if bacteria enter an open wound on another person.
Therefore, good hygiene and covering wounds are essential for prevention, particularly when dealing with infected individuals or exposed to contaminated materials.
How is Necrotizing Fasciitis diagnosed?
Diagnosis is based on clinical examination of symptoms, but the following tests can help confirm the diagnosis:
Blood tests: Such as complete blood count (CBC) and C-reactive protein (CRP) levels, along with other indicators of infection.
Tissue culture: To take a sample of the affected tissue to identify the bacteria causing the infection.
Imaging:
CT scans or MRI to assess the extent of the infection and evaluate the affected tissue.
Ultrasound may also be useful to detect fluid or gas accumulation in the tissue.
Surgical examination: A "finger test" may be performed, where tissues separate easily along the fascia, which is a strong indicator of Necrotizing Fasciitis.
What are the treatment methods for Necrotizing Fasciitis?
Immediate treatment is essential to prevent severe complications, and it includes:
Antibiotics: High doses of broad-spectrum antibiotics administered intravenously to combat the bacterial infection. A combination of antibiotics is often used to target multiple types of bacteria.
Surgery: Removal of dead tissue (debridement) is crucial to stop the infection from spreading. The patient may need several repeated surgeries to remove all affected tissue.
In severe cases, amputation of the infected limb may be necessary to save the patient's life.
Supportive treatments: These may include hyperbaric oxygen therapy, intravenous immunoglobulin (IVIG) in some cases, and wound care to accelerate healing.
Are there serious complications of Necrotizing Fasciitis?
Yes, Necrotizing Fasciitis can lead to very severe complications, including:
Sepsis (blood poisoning), a serious infection spreading throughout the bloodstream.
Septic shock, a life-threatening condition resulting from severe infection.
Multiple organ failure, affecting organs such as the kidneys, heart, and lungs.
Amputation of the affected limbs in extreme cases.
Large, permanent scars from surgery.
Death if not treated in time.
What preventive measures should be followed? Are there any tips for living with this condition after recovery?
For prevention, it is important to:
Care for cuts and scrapes, cleaning and disinfecting them to prevent bacterial entry.
Maintain body hygiene.
Avoid sharing personal items like razors or towels.
Manage chronic conditions like diabetes effectively.
After recovery, the patient may need:
Physical therapy to help rehabilitate the body.
Psychological support to deal with trauma, depression, or post-traumatic stress disorder (PTSD).
A healthy diet to promote healing.
Regular follow-up with doctors to monitor for any complications.