Health is a crown on the heads of the healthy that only the sick can see.
Is Fasting Superior to Medication in Diabetes Management?
Explore how fasting can potentially outperform medications in diabetes management. Discover the benefits, risks, and scientific insights on intermittent fasting and its effects on insulin sensitivity, particularly for type 2 diabetes patients under medical supervision.
FASTINGDIABETESGENERAL
Dr Hassan AlWarraqi
5/29/20255 min read
Is Fasting Superior to Medication in Diabetes Management?
Fasting and Diabetes: A Balanced Look at the Benefits and Medical Considerations
The idea of using fasting as a tool to manage diabetes is gaining increasing attention, with some studies highlighting potential benefits—particularly in relation to intermittent fasting and its impact on type 2 diabetes.
However, the claim that "fasting is superior to medication in treating diabetes" requires careful scrutiny.
It’s important to stress that this approach must be adopted only under strict medical supervision.
Potential Benefits of Fasting for Diabetes:
Research, especially on intermittent fasting, indicates several positive effects that could benefit individuals with type 2 diabetes,
especially in its early stages:
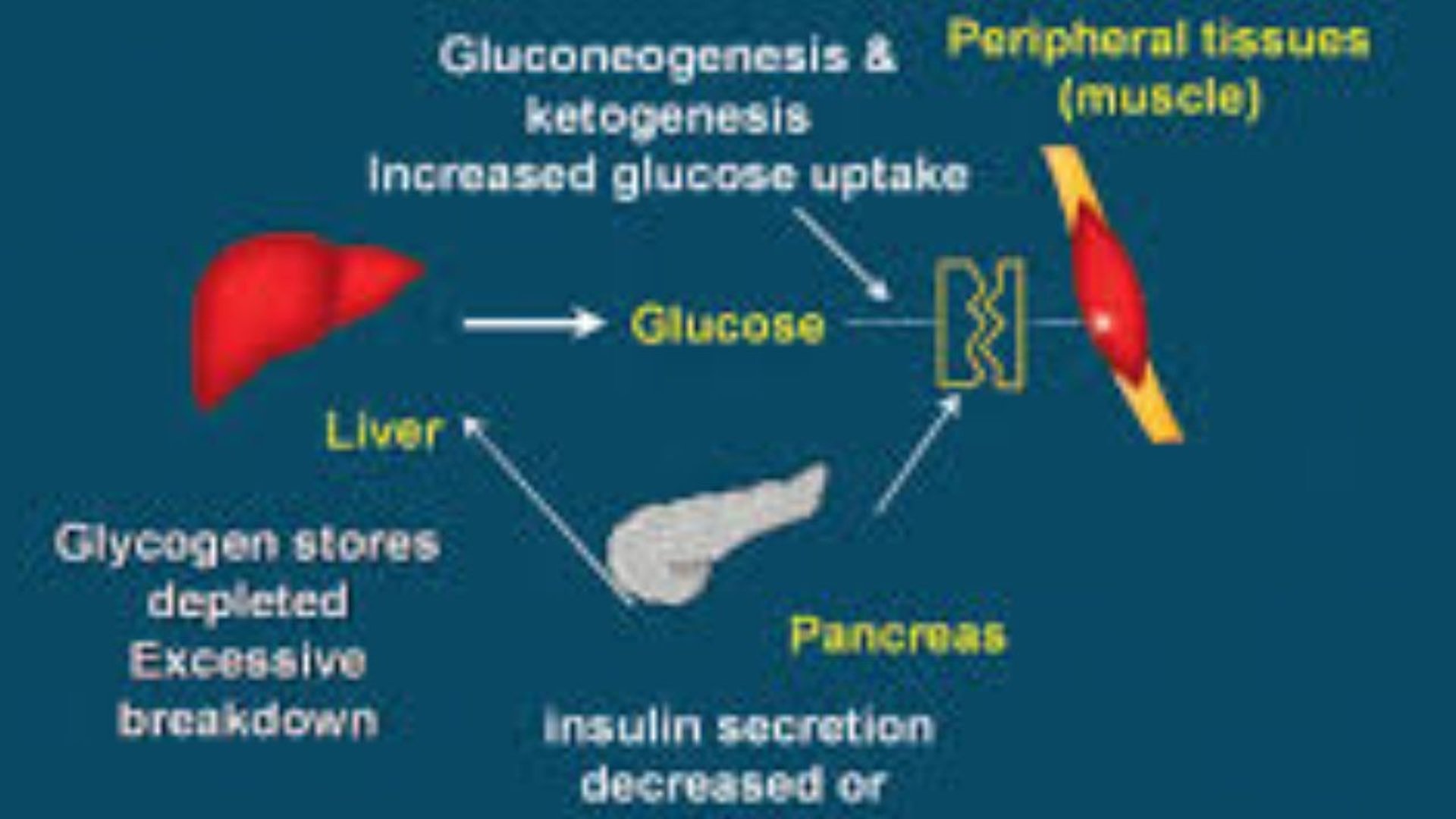
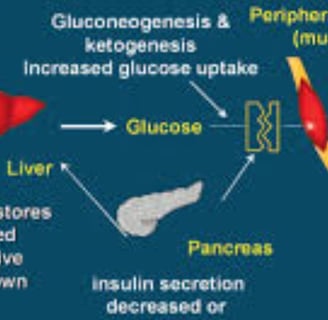
Improved Insulin Sensitivity: Fasting can reduce insulin resistance, enhancing the body's ability to use glucose effectively.
Better Blood Sugar Control: Some studies suggest that intermittent fasting—such as the 5:2 method—can be an effective lifestyle intervention in early type 2 diabetes management and may outperform some medications in such cases.
Weight Loss and Fat Reduction: Fasting contributes to weight loss and fat reduction, both crucial for better diabetes control.
Pancreatic Rest: Reduced insulin production during fasting periods may provide rest for the pancreas.
Lower Inflammation: Fasting appears to reduce markers of inflammation, which play a role in diabetes complications.
Key Medical Considerations:
Despite the potential benefits, several important points must be emphasized:
Not a Full Replacement for Medication: Fasting is not a substitute for diabetes medications.
Treatment plans depend on diabetes type, stage, overall health, and prescribed drugs.
Medical Supervision is Essential: Any diabetic patient considering fasting must consult their healthcare provider beforehand.
Only a physician can assess if fasting is appropriate and safely adjust medications, especially insulin or blood sugar-lowering drugs.
Potential Risks:
Hypoglycemia (Low Blood Sugar): The greatest risk, particularly for those on medication.
Hyperglycemia and Ketoacidosis: Especially in type 1 diabetes if insulin is not properly managed.
Dehydration and Electrolyte Imbalances
Most studies highlighting the benefits of fasting focus on type 2 diabetes in early stages, and as part of a broader lifestyle intervention.
Medications Remain a Cornerstone of
Treatment:
Global medical guidelines emphasize that medications, alongside a healthy diet and regular physical activity, are essential for diabetes management and preventing complications.
Conclusion:
Intermittent fasting shows promise as a supportive strategy in managing type 2 diabetes, potentially improving blood sugar control and insulin sensitivity—particularly when combined with a healthy lifestyle and close medical supervision.
However, considering fasting as “superior” to medication is an oversimplification that could be misleading and dangerous.
Patients must not stop or adjust their medication regimens without the full guidance of their healthcare team.
Fasting decisions must be individualized, based on comprehensive medical evaluations to ensure patient safety and achieve optimal health outcomes.
Challenges and Recommendations:
While the benefits are notable, fasting is not suitable for all diabetes patients.
Medical consultation is essential, especially for those on insulin or sulfonylureas, due to an increased risk of hypoglycemia.
Current studies mainly focus on type 2 diabetes; further research is needed for long-term outcomes and type 1 diabetes applicability.
Summary:
Evidence suggests that intermittent fasting can be an effective tool in managing early-stage type 2 diabetes and may outperform certain medications.
However, it should always be done under medical supervision and not as a full alternative to medication—particularly for patients with complex conditions.
The key challenge remains ensuring safety and tailoring fasting protocols to each individual's needs.
Insulin Resistance and Fasting,Fasting and Blood Sugar Regulation,Fasting and Insulin Sensitivity,16:8 Fasting for Diabetes,Fasting and Improving HbA1c,Intermittent Fasting and Weight Loss,Fasting and Improving Metabolism
FAQs About Fasting and Diabetes
Q: Is fasting better than medication for diabetes treatment?
A: No, fasting is not a substitute for medication. It can be a complementary therapy. Medication remains essential, and fasting may enhance its effectiveness under medical supervision.
Q: What types of fasting are suitable for diabetics?
A: The 16:8 intermittent fasting method (16 hours fasting, 8 hours eating) is generally safest for beginners. Alternate-day fasting or 24-hour fasts require stricter medical supervision.
Q: When is fasting not recommended for diabetics?
A: Avoid fasting if you have:
Uncontrolled diabetes
Frequent hypoglycemia
Advanced kidney or heart disease
Pregnancy or breastfeeding
Frailty due to old age
Q: How should I monitor blood sugar during fasting?
A: Check your blood sugar:
Before fasting
Mid-fast
When feeling unwell
Before breaking the fast
2 hours after eating
Q: What are danger signs during fasting?
A: Break your fast immediately if:
Blood sugar drops below 70 mg/dL
Blood sugar exceeds 300 mg/dL
You experience dizziness, fainting, cold sweats, tremors, chest pain, or breathing difficulty
Q: Can I reduce my medication dose while fasting?
A: Never adjust your medication without consulting your doctor. Only your physician can safely change dosages based on your tests and fasting schedule.
Q: What should I eat when breaking the fast?
A: Start with:
A small amount of water
A date or natural fruit
A balanced meal with protein and fiber
Avoid sugary foods and fried items.
Q: Does fasting cure diabetes?
A: Fasting does not cure diabetes. However, it may:
Improve insulin sensitivity
Aid in weight loss
Lower inflammation
Help stabilize blood sugar
Q: How long does it take to see results?
A: Improvements in blood sugar may appear in a few weeks. Notable changes in HbA1c take around 2–3 months.
Q: Can children with diabetes fast?
A: Children with diabetes should generally not fast, except under very specific conditions and close medical monitoring, due to their unique nutritional needs.
SEO Keywords
Fasting and diabetes, fasting effects on diabetes, intermittent fasting and type 2 diabetes, can fasting cure diabetes, fasting vs medication in diabetes treatment, benefits of fasting for diabetics, insulin resistance and fasting, fasting and blood sugar control, fasting and insulin sensitivity, 16:8 fasting for diabetics, fasting and HbA1c improvement, intermittent fasting and weight loss, fasting and metabolic health
Meta Description for SEO
Can fasting outperform medications in diabetes management? Discover the benefits, risks, and scientific insights on intermittent fasting and improved insulin sensitivity, especially for type 2 diabetes patients under medical supervision.