Fasting : Treatment of Common Long-Term Side Effects Of Covid Vaccine
Explore long covid (post-covid-19 syndrome) and its persistent symptoms like chronic fatigue, brain fog, and more. Learn about treatment options, self-care strategies, and the importance of psychological support for affected individuals, especially high-risk groups.
GENERAL
Dr Hassan Al Warraqi
4/20/202512 min read


Long COVID (Post-COVID-19 Syndrome)
a comprehensive overview of the key concepts, insights, and facts related to Long COVID, also known as Post-COVID-19 Syndrome.
It draws from diverse sources, including news reports, scientific studies, health organization recommendations, and information from treatment centers.
Definition and Scope:
Definition of Long COVID: A condition characterized by persistent or new symptoms that emerge after recovery from the initial COVID-19 infection, lasting for weeks, months, or even longer after the acute infection resolves.
Statistics: A study found that individuals infected with COVID-19 are 7.5 times more likely to meet diagnostic criteria for chronic fatigue syndrome six months post-infection compared to uninfected individuals.
WHO Definition: The condition involves symptoms that typically begin within three months of the initial COVID-19 infection and persist for at least two months.
Prevalence: Global estimates suggest approximately 6% of COVID-19 patients experience Long COVID, with millions affected since the pandemic began.
Evolution with Variants: The risk of Long COVID may have decreased with newer variants, but each new infection still carries a risk of developing the condition.
Symptom Duration: Symptoms may last from 3 to 6 months or longer, with gradual improvement typically occurring within 4-9 months, though 15% of patients experience symptoms after 12 months.
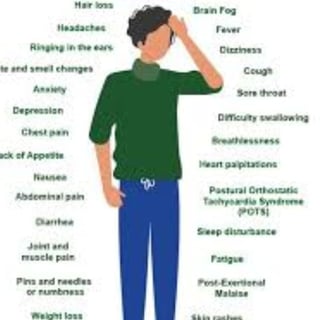
Main Symptoms:
Long COVID symptoms are highly varied, affecting multiple body systems, with over 200 different symptoms reported. Common symptoms include:
Severe Fatigue: Persistent exhaustion that hinders daily activities.
Shortness of Breath: Difficulty breathing or breathlessness, even with minimal exertion.
Brain Fog: Challenges with concentration, memory, and thinking.
Muscle and Joint Pain: Persistent pain in muscles and joints.
Sleep Disturbances: Insomnia or fragmented sleep.
Changes in Smell and Taste: Partial or complete loss of these senses.
Mood Changes: Anxiety, depression, and feelings of frustration.
Neurological Symptoms: Tremors, numbness in extremities, and unusual nighttime sensations.
Skin Symptoms: Itching, peeling skin, bruising, or unusual lumps.
Other Symptoms: Tinnitus, menstrual irregularities, digestive issues, hair loss, blurred vision, and throat problems.
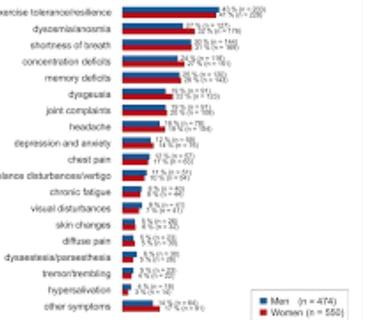
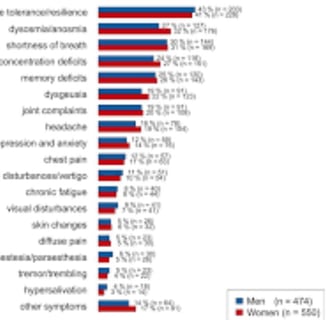
High-Risk Groups:
Long COVID can affect anyone, regardless of the severity of the initial infection.
Higher-Risk Groups Include:
Women.
Older adults.
Smokers.
Individuals with obesity or chronic conditions (e.g., diabetes, heart disease).
Those with severe COVID-19 requiring hospitalization or ICU care.
People with disabilities or limited access to healthcare.
Additional Notes: White individuals, females, those aged 46-65, and rural residents are more likely to develop chronic fatigue syndrome post-COVID.
Possible Causes:
The exact cause of Long COVID remains under investigation, but potential theories include:
Persistent viral presence, with studies detecting viral proteins in the blood of some patients.
Immune system changes or autoimmunity.
Microscopic blood clots.
Organ damage during the acute infection.
Psychological and mental factors related to post-traumatic stress.
Diagnosis and Assessment:
No Specific Test: Diagnosis relies on evaluating symptoms and medical history.
Possible Tests:
Blood tests (complete blood count, inflammation markers, clotting factors).
Kidney and liver function tests.
Imaging tests (X-rays, CT scans, MRIs) for heart, lungs, brain, or other organs as needed.
In Germany: Comprehensive imaging is conducted in Long COVID clinics to determine precise treatment paths.
Treatment and Rehabilitation:
No Specific Treatment: Management focuses on symptom relief and improving quality of life.
Strategies Include:
Self-Care: Adequate rest, sleep, healthy diet, stress management, and gradual return to physical activity.
Symptomatic Treatment: Medications for pain, anxiety, or depression.
Rehabilitation:
Pulmonary: Breathing exercises and physical therapy to improve lung function.
Neurological: Therapy to enhance memory, concentration, and stress management, including yoga and acupuncture.
Cardiac: Gradual exercise, nutritional counseling, and lifestyle adjustments.
Psychological Support: Individual or group therapy for anxiety, depression, and related emotions.
Regular Medical Follow-Up: Monitoring symptoms and adjusting treatment plans.
In Germany: Comprehensive rehabilitation programs aim to address disease consequences and enhance patient quality of life.
Fasting and Long COVID:
Studies suggest regular fasting may reduce COVID-19 complications by disrupting targeted immune cells and boosting others, limiting viral spread.
Another study on prolonged fasting in Long COVID patients showed reduced blood glucose, improved lipid profiles, and decreased inflammation, though results were inconsistent.
Vaccination and Prevention:
Vaccines reduce the likelihood of developing Long COVID.
Preventive measures include mask-wearing, personal hygiene, and proper ventilation in high-risk settings.
Link to Chronic Fatigue Syndrome (ME/CFS):
Significant overlap exists between Long COVID and ME/CFS, with 13-58% of Long COVID patients meeting ME/CFS diagnostic criteria.
The two conditions may be related or driven by similar factors.
Post-Vaccination Syndrome:
Some individuals receiving COVID-19 vaccines report symptoms resembling Long COVID, with immune changes and persistent viral proteins noted.
These findings require further research for validation.
Social and Cultural Impacts:
Acute COVID-19 is more severe in certain ethnic minorities, older adults, and low-income groups.
Long COVID affects individuals from diverse social and cultural backgrounds.
Conclusion:
Long COVID is a complex, multifaceted condition affecting a significant portion of COVID-19 survivors, with diverse, long-lasting symptoms that impact quality of life.
Research continues to uncover causes and develop effective treatments, while current management focuses on symptom relief and rehabilitation.
Vaccination and preventive measures remain critical to reducing the risk of Long COVID.
Long COVID, Chronic Fatigue Syndrome, and Prolonged Voluntary Fasting
This section examines the relationship between Long COVID (Post-COVID-19 Syndrome), Chronic Fatigue Syndrome (ME/CFS), and the potential role of prolonged voluntary fasting as a strategy to alleviate symptoms.
The content is based on scientific studies, health organization recommendations, and analysis of the overlap between these conditions.
1. Long COVID and Chronic Fatigue Syndrome: An Overview
Definition:
Long COVID: A condition characterized by persistent or new symptoms following recovery from COVID-19, such as severe fatigue, brain fog, shortness of breath, and muscle pain, lasting weeks or months.
Chronic Fatigue Syndrome (ME/CFS): A chronic disorder marked by unexplained severe fatigue, post-exertional malaise (PEM), sleep disturbances, and cognitive impairments.
Overlap:
There is significant similarity between Long COVID and ME/CFS, particularly in chronic fatigue, brain fog, and symptom worsening after activity.
Estimates suggest 13-58% of Long COVID patients meet ME/CFS diagnostic criteria.
A study found that COVID-19 patients are 7.5 times more likely to develop ME/CFS-like symptoms six months post-infection compared to non-infected individuals.
Shared Symptoms:
Chronic fatigue, brain fog, post-exertional malaise, sleep disturbances, muscle and joint pain, and mood changes (e.g., anxiety, depression).
Additional Long COVID Symptoms: Changes in smell/taste, shortness of breath, skin symptoms (e.g., itching), and neurological symptoms (e.g., tremors).
High-Risk Groups
Long COVID: Women, older adults, smokers, individuals with obesity or chronic conditions, and those with severe COVID-19 requiring ICU care.
ME/CFS Post-COVID: White women, ages 46-65, rural residents, and those less likely to be vaccinated or have completed college education.
Possible Causes
Persistent viral presence or viral proteins in the body.
Immune dysfunction or autoimmunity.
Chronic inflammation or microscopic blood clots.
Organ damage during acute infection.
Metabolic disruptions or reactivation of latent viruses (e.g., Epstein-Barr).
Psychological factors, such as chronic stress or trauma.
2. Prolonged Voluntary Fasting: Its Role and Impact
Definition of Prolonged Voluntary Fasting
Prolonged voluntary fasting involves abstaining from food for extended periods (typically over 24 hours), such as intermittent fasting or multi-day fasting, while consuming water and non-caloric fluids.
Relationship with Long COVID and ME/CFS
Studies suggest fasting may influence immune responses, inflammation, and energy metabolism, which are relevant to both Long COVID and ME/CFS.
Study on Fasting and COVID-19
Found that regular fasting may reduce COVID-19 complications by disrupting T-cells targeted by the virus, boosting other immune cells, and limiting viral spread.
Study on Fasting and Long COVID
Demonstrated improvements in some parameters for Long COVID patients, including:
Reduced blood glucose levels.
Improved lipid profiles (e.g., cholesterol).
Decreased inflammatory markers (e.g., cytokines).
However, changes in inflammatory markers were inconsistent across patients, indicating a need for further research.
Fasting and ME/CFS
No direct studies link prolonged fasting to ME/CFS, but theoretically, fasting could reduce chronic inflammation or enhance mitochondrial function (cellular energy production), which are implicated in ME/CFS.
Caution is needed, as prolonged fasting may exacerbate fatigue or PEM in ME/CFS patients if not carefully managed.
Mechanisms of Fasting
Autophagy: Fasting triggers autophagy, where cells remove damaged components, potentially reducing inflammation and supporting tissue repair.
Immune Modulation: Fasting reduces overactive immune responses and promotes immune balance.
Reduced Oxidative Stress: May mitigate cellular damage from chronic inflammation.
Challenges and Risks
Long COVID: Fasting may not suit all patients, especially those with nutritional deficiencies or metabolic issues.
ME/CFS: ME/CFS patients are highly sensitive to energy fluctuations, and prolonged fasting could worsen symptoms without medical supervision.
Need for Supervision: Prolonged fasting should be conducted under medical guidance to ensure adequate nutrition and avoid complications like hypoglycemia or dehydration.
3. Diagnosis and Treatment
Diagnosis:
Long COVID: Relies on medical history and symptom assessment, with tests (e.g., blood work, imaging) to rule out other causes.
ME/CFS: Based on diagnostic criteria (e.g., IOM criteria), requiring chronic fatigue for over 6 months, PEM, and additional symptoms like poor sleep or brain fog.
Challenge: Overlap between the conditions complicates diagnosis, especially with limited specific biomarkers.
Treatment and Rehabilitation:
Long COVID:
Self-Care: Rest, healthy diet, stress management.
Symptomatic Treatment: Medications for pain, anxiety, or depression.
Rehabilitation: Breathing exercises, cognitive therapy, and pulmonary or neurological programs.
ME/CFS:
Activity Management (Pacing): Energy allocation to avoid PEM.
Cognitive Behavioral Therapy (CBT): To improve symptom management, not as a cure.
Multidisciplinary Support: Neurologists, psychologists, and rehabilitation specialists.
Fasting as a Potential Treatment
Prolonged fasting may serve as a complementary intervention to reduce inflammation and improve metabolic parameters but is not a standard treatment.
Requires tailored fasting protocols under medical supervision, especially for ME/CFS patients.
4. Prevention and Recommendations
Vaccination: Reduces Long COVID risk and may alleviate symptoms in some cases.
Preventive Measures: Mask-wearing, hygiene, and ventilation to minimize COVID-19 infection.
Fasting: May have potential as a preventive strategy to reduce COVID-19 complications, but more studies are needed to confirm its efficacy for Long COVID and ME/CFS.
ME/CFS Management: Reducing viral infections and stress may help prevent symptom exacerbation.
5. Social Impacts
Long COVID: Affects diverse groups, with higher risks for ethnic minorities and those in areas with limited healthcare access.
ME/CFS: Often misunderstood, leading to social stigma and challenges in accessing medical support.
Fasting: May face cultural or social barriers, particularly if tied to religious or health beliefs.
Conclusion:
Long COVID and Chronic Fatigue Syndrome share significant overlap in symptoms and potential biological mechanisms, such as chronic inflammation and immune dysfunction.
Prolonged voluntary fasting shows promise as a complementary intervention to reduce inflammation and improve metabolic markers in Long COVID, but it requires careful medical supervision, particularly for ME/CFS patients who are sensitive to energy changes.
Ongoing research is needed to clarify the relationship between these conditions and develop effective treatment strategies, while vaccination and preventive measures remain critical to reducing Long COVID risks.
FAQs: Long COVID, Chronic Fatigue Syndrome (ME/CFS), and Prolonged Voluntary Fasting
1. What is Long COVID, and how does it differ from Chronic Fatigue Syndrome (ME/CFS)?
Long COVID refers to a range of persistent or new symptoms that continue for weeks, months, or longer after recovering from the initial COVID-19 infection. Common symptoms include fatigue, brain fog, shortness of breath, and muscle pain.
Chronic Fatigue Syndrome (ME/CFS) is a chronic condition characterized by severe, unexplained fatigue lasting over six months, post-exertional malaise (PEM, symptom worsening after activity), sleep disturbances, and cognitive issues.
Key Difference: Long COVID is specifically tied to a prior COVID-19 infection and may include symptoms like loss of smell/taste or respiratory issues, while ME/CFS can occur without a clear viral trigger.
However, 13-58% of Long COVID patients meet ME/CFS diagnostic criteria, indicating significant overlap.
2. What are the common symptoms shared between Long COVID and ME/CFS?
Both conditions share several symptoms, including:
Chronic Fatigue: Persistent exhaustion that doesn’t improve with rest.
Brain Fog: Difficulty with concentration, memory, and decision-making.
Post-Exertional Malaise (PEM): Worsening symptoms after physical or mental effort.
Sleep Disturbances: Insomnia, unrefreshing sleep, or fragmented sleep.
Muscle and Joint Pain: Persistent pain without a clear cause.
Mood Changes: Anxiety, depression, or frustration.
Long COVID may also involve unique symptoms like shortness of breath, changes in smell/taste, and skin or neurological issues (e.g., tremors).
3. Who is at higher risk for developing Long COVID or ME/CFS after COVID-19?
Long COVID:
Women, older adults, smokers, individuals with obesity, or chronic conditions (e.g., diabetes, heart disease).
Those with severe COVID-19 requiring hospitalization or ICU care.
People in areas with limited healthcare access.
ME/CFS Post-COVID:
White women, ages 46-65, living in rural areas.
Individuals less likely to be vaccinated or have completed college education.
A study found that COVID-19 patients are 7.5 times more likely to develop ME/CFS-like symptoms six months post-infection compared to non-infected individuals.
4. What causes Long COVID and ME/CFS, and are they related?
The exact causes are still under investigation, but potential factors include:
Persistent Viral Presence: Viral proteins lingering in the body.
Immune Dysfunction: Abnormal immune responses or autoimmunity.
Chronic Inflammation: Elevated inflammatory markers like cytokines.
Organ Damage: Tissue damage from acute infection.
Metabolic Issues: Disruptions in cellular energy production.
Psychological Factors: Chronic stress or trauma.
Relationship: The overlap in symptoms and potential mechanisms (e.g., inflammation, immune dysregulation) suggests Long COVID and ME/CFS may share underlying biological pathways. Some researchers hypothesize they could be triggered by similar factors, such as viral infections or immune overactivation.
5. How are Long COVID and ME/CFS diagnosed?
Long COVID:
Diagnosed based on medical history and symptom assessment, as there is no specific test.
Tests like blood work (e.g., inflammation markers) or imaging (e.g., CT scans) may rule out other causes.
ME/CFS:
Diagnosed using criteria like the Institute of Medicine (IOM) guidelines, requiring chronic fatigue for over six months, PEM, and additional symptoms (e.g., unrefreshing sleep, cognitive issues).
Other conditions (e.g., thyroid disorders) must be ruled out.
Challenge: Overlap in symptoms and lack of specific biomarkers make diagnosis complex for both conditions.
6. What is prolonged voluntary fasting, and how might it help with Long COVID or ME/CFS?
Prolonged Voluntary Fasting involves abstaining from food for extended periods (e.g., over 24 hours), such as intermittent fasting or multi-day fasting, while consuming water and non-caloric fluids.
Potential Benefits:
For Long COVID:
A study found regular fasting may reduce COVID-19 complications by disrupting virus-targeted T-cells and limiting viral spread.
Another study showed fasting improved blood glucose, lipid profiles, and some inflammatory markers in Long COVID patients, though results were inconsistent.
For ME/CFS:
No direct studies, but fasting may reduce chronic inflammation or enhance mitochondrial function, potentially alleviating symptoms.
Mechanisms include autophagy (cellular cleanup), immune modulation, and reduced oxidative stress.
Caution: Fasting may worsen fatigue or PEM, especially in ME/CFS patients, and should only be attempted under medical supervision.
7. What are the risks of prolonged fasting for Long COVID or ME/CFS patients?
Long COVID: Fasting may not be suitable for those with nutritional deficiencies or metabolic disorders, risking complications like hypoglycemia or dehydration.
ME/CFS: Patients are highly sensitive to energy changes, and prolonged fasting could exacerbate fatigue or PEM without careful management.
General Risks: Potential for nutrient deficiencies, electrolyte imbalances, or worsening symptoms if fasting is not properly supervised.
Medical guidance is essential to tailor fasting protocols and ensure safety.
8. How are Long COVID and ME/CFS treated?
Long COVID:
Self-Care: Adequate rest, healthy diet, stress management, and gradual physical activity.
Symptomatic Treatment: Medications for pain, anxiety, or depression.
Rehabilitation:
Pulmonary: Breathing exercises to improve lung function.
Neurological: Cognitive therapy, yoga, or relaxation techniques.
Cardiac: Gradual exercise and lifestyle changes.
Psychological Support: Therapy for anxiety or depression.
ME/CFS:
Pacing: Managing energy to avoid PEM.
Cognitive Behavioral Therapy (CBT): To improve symptom coping, not as a cure.
Medications: Antidepressants or sleep aids in some cases.
Multidisciplinary Care: Involving neurologists, psychologists, and rehabilitation specialists.
Note: Avoid strenuous exercise in both conditions to prevent symptom worsening. Comprehensive rehabilitation programs, like those in Germany, focus on improving quality of life.
9. Can fasting be used as a treatment for Long COVID or ME/CFS?
Fasting is not a standard treatment but may serve as a complementary approach:
Long COVID: Preliminary studies suggest fasting could reduce inflammation and improve metabolic markers, but it’s not a cure and requires further research.
ME/CFS: No direct evidence supports fasting as a treatment, and it may worsen symptoms in some patients due to energy demands.
Fasting should be personalized and medically supervised, especially for ME/CFS patients.
10. How can Long COVID and ME/CFS be prevented?
Long COVID:
Vaccination: Reduces the risk of Long COVID and may alleviate symptoms.
Preventive Measures: Mask-wearing, hygiene, and proper ventilation to avoid COVID-19 infection.
ME/CFS:
No direct prevention, but reducing viral infections and managing stress may lower the risk of triggering or worsening symptoms.
Fasting: May have a preventive role by reducing COVID-19 complications, but more studies are needed.
11. What are the social impacts of Long COVID and ME/CFS?
Long COVID: Affects diverse populations, with higher risks for ethnic minorities, older adults, and those with limited healthcare access. It can impair work and daily life.
ME/CFS: Often misunderstood, leading to social stigma, delayed diagnosis, and challenges accessing medical support.
Fasting: May face cultural or social barriers, especially if tied to religious or health practices.
12. Are there ongoing research efforts for Long COVID, ME/CFS, and fasting?
Yes, research is active in:
Understanding the biological mechanisms of Long COVID and ME/CFS, including inflammation and immune dysregulation.
Exploring fasting’s effects on inflammation, metabolism, and immune function in Long COVID.
Developing targeted treatments and diagnostic tools for both conditions.
Continued studies are needed to confirm fasting’s efficacy and safety for Long COVID and ME/CFS.
keywords
Long COVID, Post-COVID-19 Syndrome, persistent COVID symptoms, chronic fatigue, brain fog, shortness of breath, muscle pain, sleep disturbances, loss of smell and taste, mood changes, neurological symptoms, skin symptoms, Chronic Fatigue Syndrome, ME/CFS, post-exertional malaise, chronic inflammation, autoimmunity, microscopic blood clots, viral persistence, prolonged voluntary fasting, autophagy, immune modulation, reduced oxidative stress, vaccination, preventive measures, rehabilitation, symptomatic treatment, self-care, psychological support, social impacts, high-risk groups, women, older adults, obesity, chronic diseases, limited healthcare access areas, diagnosis, blood tests, imaging tests, comprehensive rehabilitation programs, Germany, scientific research, World Health Organization, variants, Long COVID prevalence, symptom duration, gradual improvement
can long covid come and go can long covid symptoms be delayed covid and long covid symptoms for how long covid patient is infectiou show long post covid syndrome last