Effects Of Fasting On Multiple Sclerosis : remyelination
Explore the complex relationship between multiple sclerosis and Islamic fasting. Learn about symptoms, treatment options, the role of the gut microbiome, and how autophagy can help decrease inflamm...
NERVOUS SYSTEM
Dr Hassan Alwarraqi
9/13/20248 min read


ms and fasting
what is multiple sclerosis
Multiple sclerosis (MS) is a long-term illness that affects the central nervous system.
The disease is characterized by its unpredictability;
Some individuals may be only slightly impacted, while others may lose their ability to see clearly, write, speak, or walk.
Early signs can include issues with vision, difficulties in walking, and sensations of tingling
Multiple sclerosis (MS) is a condition that occurs when the immune system attacks the central nervous system, specifically the brain and spinal cord.
Common symptoms include visual issues, fatigue, difficulties with walking and balance, as well as numbness or weakness in the extremities.
The underlying causes of MS remain unknown,
but a family history of the disease may heighten the risk of its development
While there is no known cure for MS, treatment options are available that can alleviate symptoms, prevent further relapses, and enhance the quality of life for patients
It disrupts cognitive, emotional, motor, sensory, and visual functions due to the immune system's attack on the brain and spinal cord.
It is estimated that over 1.8 million people are affected by MS worldwide
it can occur in individuals of all ages, it is particularly common among young adults and women.
Early treatment with medications can enhance or stabilize the condition
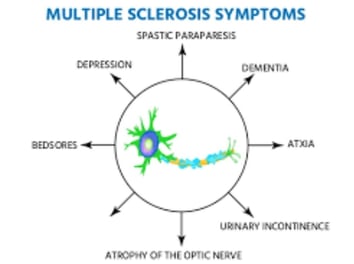
multiple sclerosis symptoms
The manifestation of multiple sclerosis symptoms can be aggravated by heat or during the occurrence of other infections,
such as urinary tract or respiratory infections. Symptoms may present as: problems with vision, challenges in ambulation or balance, cognitive difficulties, numbness or weakness
primarily in the arms and legs, muscle rigidity, depressive symptoms, issues with sexual function or urination, significant fatigue, sensory loss, speech issues, tremors, and dizziness
depression may happen
Problems with sexual, bowel and bladder function
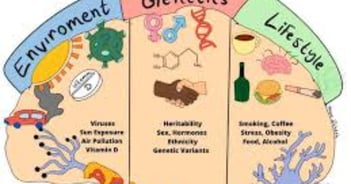
multiple sclerosis cause
The risk factors for multiple sclerosis (MS) are not yet fully defined.
that the disease may develop when specific genetic mutations are influenced by environmental conditions.
This situation is not simply a result of unfavorable genes or a negative environment; rather,
it is the problematic interaction between genetic factors and environmental influences that is significant
Dietary Habits. An unhealthy dietary pattern that is rich in salt and fats is considered to promote inflammation throughout the body,
thereby serving as a potential risk factor for the onset of multiple sclerosis (MS).
Cigarette Smoking. strong correlation between smoking and increased rates of MS.
Heavy smokers, specifically those who smoke over four packs daily, are five times more likely to develop MS than their non-smoking counterparts.
Additionally, for patients with existing relapse-remitting MS, smoking more than ten cigarettes each day is associated with an increased risk of progression to secondary progressive MS
causes & symptoms multiple sclerosis in females
Although the incidence of MS is higher in females compared to males, the symptoms tend to be similar across genders.
females may experience distinct variations in their symptoms due to hormonal differences and fluctuations, particularly during menstrual cycles, pregnancy, or menopause.
The initial manifestations of MS often include visual impairments and patchy numbness. Other prevalent symptoms include depression, urinary issues, cognitive changes, and pain.
Currently, there is no cure for MS; however, a variety of medications and complementary therapies are typically effective in managing symptoms and may help to slow the progression of the disease
Types of multiple sclerosis
five distinct courses:
Clinically isolated syndrome is characterized by symptoms arising from a single episode, also known as an exacerbation or relapse, followed by a complete or nearly complete recovery.
Diagnostic imaging, such as magnetic resonance imaging (MRI), along with other assessments like spinal taps or visual evoked potentials, may reveal "silent" lesions in other areas of the central nervous system.
The identification of such damage can facilitate a definitive diagnosis of MS, even after just one episode.
Relapsing-remitting MS is marked by recurrent episodes of symptoms, with either total or partial recovery following each attack. The intervals of inactivity between these episodes are termed remission, which can last for weeks, months, or even years before another attack occurs.
Disease-modifying therapies are available to decrease the frequency of these attacks or potentially eliminate them altogether.
Secondary-progressive MS may develop from relapsing-remitting MS, leading to a gradual worsening of symptoms and a decline in functional abilities over time.
This type can be classified as "active" if it includes attacks, or "non-relapsing" if it does not.
Primary-progressive MS is a less prevalent form that is characterized by a continuous progression of symptoms from the onset,
without any distinct acute attacks, although there may be brief periods of symptom exacerbation or relief.
Radiologically isolated syndrome represents the rarest form of MS, where individuals exhibit abnormal MRI findings suggestive of MS but do not present any clinical symptoms.
Nonetheless, there is a possibility that symptoms may manifest in the future
multiple sclerosis diagnosis
its not accomplished through a single test. Instead, healthcare professionals utilize a range of evaluations to either confirm or rule out the condition. In addition to gathering a thorough medical history, conducting a physical examination, and performing a detailed neurological assessment, a physician may recommend MRI scans of the brain and spinal cord to detect the typical lesions indicative of MS. An intravenous injection of a contrast agent may be utilized to enhance the imaging results.
Additionally, a physician may suggest:
A lumbar puncture,
also known as a spinal tap, to collect cerebrospinal fluid for analysis, which can reveal proteins and inflammatory cells associated with MS.
This procedure can also help differentiate other conditions that may present similarly to MS.
Evoked potential tests, which involve the placement of electrodes on the skin and the application of painless electrical signals to evaluate the responsiveness and speed of the nervous system to stimuli.
MRI of the optic nerves, optical coherence tomography (OCT), or visual evoked potentials to identify lesions affecting the optic nerve
multiple sclerosis treatment
Each person's treatment plan for multiple sclerosis (MS) is unique,
shaped by the disease's stage and the symptoms they encounter.
To combat fatigue, a common issue for many with MS, individuals might implement strategies such as
regular exercise, fostering healthy sleep patterns, and avoiding medications that could worsen fatigue
The approach to treating multiple sclerosis (MS) involves two key elements:
immunomodulatory therapy (IMT), which targets the fundamental immune disorder, and
therapies intended to relieve or alter symptoms. IMT is primarily concerned with minimizing relapse frequency and hindering disease progression.
Furthermore, Mitoxantrone is approved for use in secondary progressive and progressive-relapsing MS
Corticosteroids, such as methylprednisolone
Natalizumab (brand name: Tysabri
Ocrelizumab (brand name: Ocrevus®)
Alemtuzumab
Injectable medication
Beta interferon
side effects of these drugs include flu-like symptoms , depression, or elevation of liver enzymes.
Glatiramer acetate
multiple sclerosis and fasting
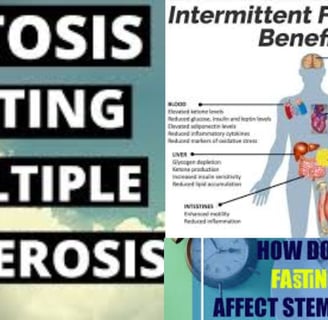
Intermittent fasting encompasses several methods that are utilized today for diverse purposes, including the enhancement of health.
Recent investigations have revealed encouraging outcomes regarding the effects of intermittent fasting on the symptoms and progression of multiple sclerosis (MS).
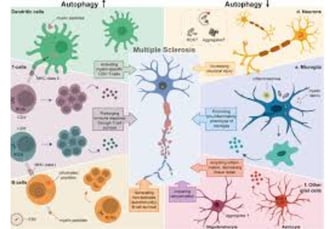
It is hypothesized that this practice aids in the equilibrium of gut microbiota, which may subsequently diminish inflammation throughout the body
islamic fasting
muslims with ms
gut microbion
autophagy
decrease inflammation
control sugar insulin resistance
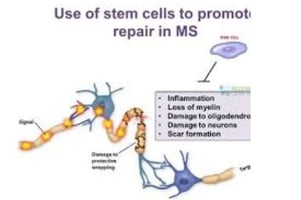
increased stem cell
ketosis
references
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3994348/
https://www.sciencedirect.com/science/article/abs/pii/S2211034823006843
https://mscanada.ca/find-support/blog/on-faith-fasting-being-a-muslim-living-with-multiple-sclerosis
https://www.reddit.com/r/MultipleSclerosis/comments/1asq4kp/ramadan/
https://www.hopkinsmedicine.org/health/conditions-and-diseases
https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
keywords
multiple sclerosis ,symptoms,muslims with ms,gut microbiome , autophagy ,decrease inflammation ,control sugar insulin resistance,increased stem cell,islamic fasting,intermittent fasting , treatment ,diagnosis , investigations ,types , radiology , mri , unpredictability ,the immune system attacks,central nervous system, the brain , spinal cord ,causes of MS , unknown,
Questions and Answers about Multiple Sclerosis (MS) and Fasting
What is Multiple Sclerosis (MS) and how does it affect the body?
Multiple Sclerosis (MS) is a chronic disease that affects the central nervous system (brain and spinal cord).
It occurs when the body’s immune system attacks the protective substance (myelin) covering nerve fibers.
This attack causes inflammation and nerve damage, leading to a variety of symptoms, including vision problems, difficulty walking and balancing, fatigue, numbness or weakness in the limbs, cognitive issues, mood swings, and bowel/bladder dysfunction.
MS is an unpredictable disease, with symptom severity and impact varying widely between individuals.
What are the causes and risk factors for developing MS?
The exact causes of MS remain unknown, but it is believed to result from a complex interaction between genetic and environmental factors.
A family history of MS increases the risk. Environmental factors such as smoking and unhealthy diets high in salt and fats may also play a role by promoting inflammation.
MS is not directly caused by unfavorable genes or a negative environment alone but by their interaction.
What are the different types of MS, and how do they progress?
There are several types of MS, each with a distinct progression:
Clinically Isolated Syndrome (CIS): A single episode of symptoms with full or partial recovery. MRI may show additional "silent" lesions.
Relapsing-Remitting MS (RRMS): Characterized by recurrent symptom flare-ups followed by recovery periods.
Secondary Progressive MS (SPMS): Develops from RRMS, leading to gradual worsening of symptoms over time.
Primary Progressive MS (PPMS): Continuous symptom progression from onset, without clear acute attacks.
Radiologically Isolated Syndrome (RIS): Abnormal MRI findings without clinical symptoms.
How is MS diagnosed?
No single test diagnoses MS. Diagnosis relies on a combination of assessments:
Medical history, physical, and neurological exams to evaluate symptoms and neurological function.
MRI scans of the brain and spinal cord to detect MS-related lesions.
Lumbar puncture (spinal tap) to analyze cerebrospinal fluid for inflammatory proteins/cells.
Evoked potential tests to assess nervous system response to stimuli.
Vision tests, including optical coherence tomography (OCT) and visual evoked potentials.
What treatment options are available for MS?
There is no cure for MS, but treatments aim to manage symptoms, slow progression, and improve quality of life:
Disease-modifying therapies (DMTs): Reduce relapses and delay progression (e.g., interferon beta, glatiramer acetate, oral/injectable medications).
Corticosteroids: Used for acute flare-ups.
Other medications: Mitoxantrone, natalizumab, ocrelizumab, alemtuzumab.
Symptom management: Treatments for fatigue, pain, spasms, etc.
Complementary therapies: May help improve symptoms.
What is fasting, and how might it affect people with MS?
Fasting involves alternating periods of normal eating with severe calorie restriction.
Types include time-restricted eating, the 5:2 diet, fasting-mimicking diets, and alternate-day fasting.
Preliminary research suggests fasting may improve MS symptoms by calming the overactive immune response that damages nerves, reducing inflammation, and improving gut bacteria balance.
What do recent studies say about fasting’s impact on MS?
Animal studies show fasting may reduce inflammation, myelin damage, and MS-like symptoms.
In one mouse study, fasting led to lower inflammatory cytokines, less myelin damage, and milder symptoms.
Other studies noted increased beneficial gut bacteria.
Early human trials show promise, but larger studies are needed to confirm long-term benefits.
What precautions should people with MS take before trying fasting?
Consult a doctor first, as fasting may not suit everyone.
Potential side effects include blood sugar fluctuations, constipation, low energy, and bad breath.
Ensure adequate nutrient intake during eating periods.
Fasting is not a primary treatment for MS but should complement a holistic approach, including standard therapies, a healthy diet, and exercise.