Cardiac Catheterization: Why Every Case Is Followed by a Stent
Discover why cardiac catheterization is often followed by stent placement. Learn about the procedures, types of stents, and their importance in treating coronary artery disease and acute coronary syndrome. Understand the recovery process and how these interventions improve heart health.
CARDIOVASCULAR
Dr Hassan AlWarraqi
12/30/2024


Cardiac Catheterization: Why Every Case Is Followed by a Stent
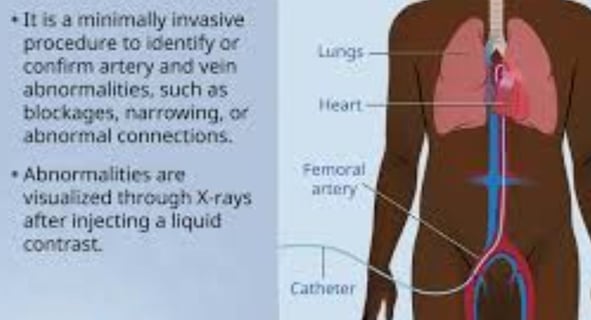
Cardiac catheterization is a vital medical procedure used to diagnose and treat various heart conditions
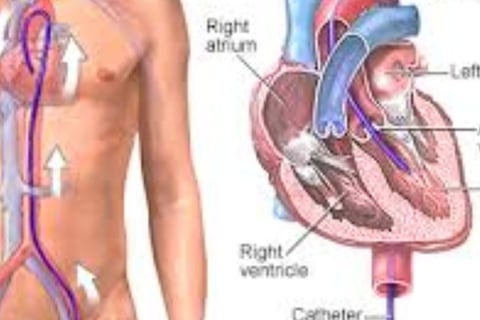
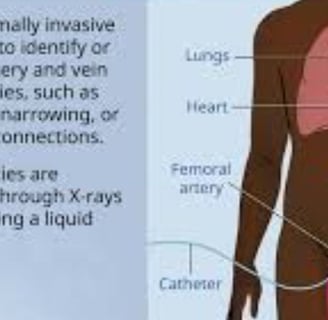
It involves inserting a thin, flexible tube (catheter) into a blood vessel, typically in the arm or groin, and guiding it to the heart.
While this procedure is essential for identifying heart issues, not every case results in stent placement.
Here’s a detailed look at why stents are not always used and when they are necessary.
Cardiac catheterization serves two primary purposes:
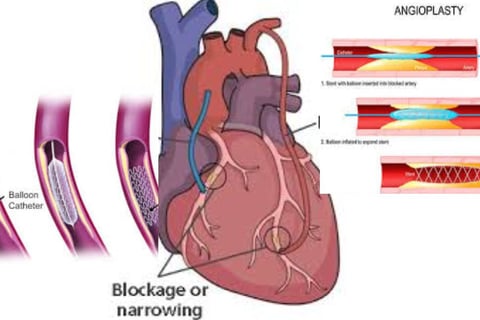
Diagnosis: It helps detect blocked or narrowed coronary arteries, measures heart chamber pressures, evaluates heart function, and assesses heart valve conditions.
Treatment: It allows for procedures like angioplasty (to open blocked arteries) or stent placement to restore blood flow.
Preparation for Cardiac Catheterization
Proper preparation ensures a safe and successful procedure:
Fasting: Avoid eating or drinking for 6–8 hours before the procedure.
Medication Review: Inform your doctor about all medications, especially blood thinners or diabetes medications.
Allergy Check: Notify your doctor of any allergies, particularly to iodine, contrast dye, or latex.
Health Assessment: Discuss recent illnesses, infections, or kidney problems, as contrast dye can affect kidney function.
Types of Treatments During Cardiac Catheterization
Depending on the findings, treatments may include:
Angiography: Visualizing blockages using contrast dye.
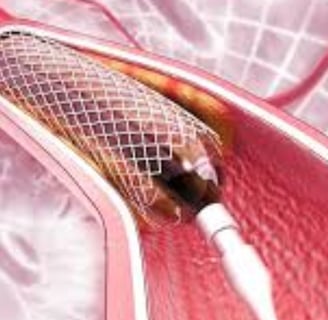
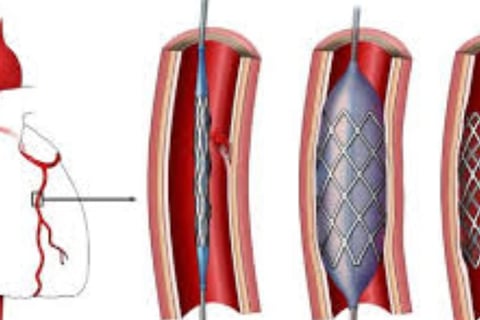
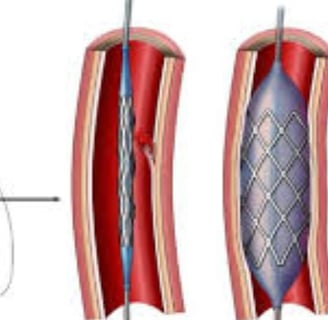
Angioplasty and Stent Placement: Widening blocked arteries and inserting stents to keep them open.
Thrombectomy: Removing clots in cases of acute heart attack.
Valve Assessment or Repair: Evaluating or repairing heart valves.
Other Procedures: Atherectomy (plaque removal) or electrophysiology studies for heart rhythm issues.
Recovery After Cardiac Catheterization
Recovery varies based on whether the procedure was diagnostic or therapeutic:
Immediate Recovery: Monitoring vital signs and the insertion site.
Returning Home: Most diagnostic procedures allow same-day discharge, while stent placement may require an overnight stay.
Post-Procedure Care: Avoid strenuous activity, keep the insertion site clean, and adhere to prescribed medications.
Percentage of Cardiac Catheterizations Ending with Stent Placement
The likelihood of stent placement depends on several factors:
General Statistics: 30%–50% of cardiac catheterizations for chest pain result in stent placement.
Severity of Blockage: Stents are typically used for blockages of 70% or more.
Type of Chest Pain: Acute coronary syndromes (e.g., heart attacks) are more likely to require stents than stable chest pain.
Diagnostic Findings: Non-invasive tests suggesting significant ischemia increase the likelihood of stenting.
Why Every Case Is Not Followed by a Stent
Stents are not always necessary.
Here’s why:
No Significant Blockage: Healthy or mildly narrowed arteries do not require stents.
Medical Management: Medications and lifestyle changes can manage some blockages.
Bypass Surgery: Severe or complex blockages may need coronary artery bypass grafting (CABG).
Non-Coronary Issues: Procedures for valve disease or congenital defects do not involve stents.
Stents are typically placed in the following scenarios:
Coronary Artery Disease (CAD): Significant blockages (>70% narrowing) in the coronary arteries.
Acute Coronary Syndrome (ACS): Heart attacks or unstable angina requiring immediate intervention.
Symptomatic Relief: Alleviating chest pain (angina) caused by reduced blood flow.
Preventive Measure: Reducing the risk of future heart attacks or complications.
Types of Stents
Bare-Metal Stents (BMS): Basic metal scaffolds.
Drug-Eluting Stents (DES): Coated with medication to prevent re-narrowing.
Bioresorbable Stents: Temporary stents that dissolve over time.
Conclusion
While stents are commonly used after cardiac catheterization, they are not required in every case.
The decision depends on the severity and location of blockages, the patient’s symptoms, and overall health.
The ultimate goal is to improve blood flow to the heart and reduce the risk of heart attacks or other complications.
Keywords in Sequence:
Cardiac Catheterization, Stent Placement, Angioplasty, Coronary Artery Disease, Acute Coronary Syndrome, Angiography, Bare-Metal Stents, Drug-Eluting Stents, Bioresorbable Stents, Heart Health, Chest Pain, Blocked Arteries, Heart Attack, Recovery After Catheterization.
Frequently Asked Questions About Cardiac Catheterization and Stent Placement
1. What is cardiac catheterization, and what are its primary goals?
Cardiac catheterization is a vital medical procedure involving the insertion of a thin, flexible tube (catheter) into a blood vessel, usually in the arm or groin, and guiding it to the heart.
Diagnostic Goals:
Detect blocked or narrowed coronary arteries.
Measure pressure in the heart chambers.
Evaluate heart function.
Assess heart valve conditions.
Therapeutic Goals:
Perform procedures such as angioplasty (to open blocked arteries).
Place stents to restore blood flow.
2. What preparations are necessary before undergoing cardiac catheterization?
To ensure a safe and successful procedure, the following preparations are essential:
Fasting: Avoid eating and drinking for 6–8 hours before the procedure.
Medication Review: Inform your doctor about all medications you take, especially blood thinners or diabetes medications.
Allergy Check: Notify your doctor of any allergies, particularly to iodine, contrast dye, or latex.
Health Evaluation: Discuss any recent illnesses, infections, or kidney issues, as the contrast dye can affect kidney function.
3. What treatments can be performed during cardiac catheterization?
Various treatments can be performed during cardiac catheterization depending on the findings:
Angiography: Using contrast dye to visualize blockages.
Angioplasty and Stent Placement: Widening blocked arteries and placing stents to keep them open.
Thrombectomy: Removing clots in cases of acute heart attack.
Valve Assessment or Repair: Evaluating or repairing heart valves.
Other Procedures:
Atherectomy: Removing plaque from arteries.
Electrophysiological Studies: Testing and treating heart rhythm issues.
4. How long is the recovery after cardiac catheterization, and what care is required post-procedure?
Recovery time depends on whether the procedure was diagnostic or therapeutic.
Immediate Recovery:
Vital signs and the insertion site are monitored closely.
Most diagnostic procedures allow same-day discharge.
Procedures involving stents may require an overnight stay.
Post-Procedure Care:
Avoid strenuous activities.
Keep the insertion site clean.
Follow prescribed medications, especially blood thinners.
5. What percentage of cardiac catheterizations end with stent placement?
The likelihood of stent placement depends on several factors:
Approximately 30–50% of cardiac catheterizations performed for chest pain result in stent placement.
Stents are more likely when:
Blockages are severe (≥70%).
Acute coronary syndromes (e.g., heart attacks) are present.
Non-invasive tests indicate significant ischemia.
6. Why isn’t a stent placed in every cardiac catheterization case?
Stents are not always necessary.
Mild or healthy arteries do not require stents.
Some blockages can be managed with medications and lifestyle changes.
Severe or complex blockages might require coronary artery bypass grafting (CABG).
Procedures for valve diseases or congenital defects do not involve stents.
7. When are stents necessary, and what types are available?
Stents are necessary in cases such as:
Coronary artery disease (CAD) with severe blockages (≥70%).
Acute coronary syndrome (ACS), including heart attacks or unstable angina.
Relieving chest pain caused by reduced blood flow.
Preventing future heart attacks or complications.
Types of Stents:
Bare-metal stents (BMS): Basic metal structure.
Drug-eluting stents (DES): Coated with medication to prevent re-narrowing.
Bioabsorbable stents: Designed to dissolve over time.
8. What is the ultimate goal of cardiac catheterization, whether it includes stent placement or not?
The primary goal of cardiac catheterization is to improve blood flow to the heart and reduce the risk of heart attacks or other complications.
Whether or not stents are placed, the procedure aims to accurately diagnose heart problems and provide appropriate treatment to enhance overall heart health.