
Health is a crown on the heads of the healthy that only the sick can see.
🤢 Vomiting and Obstructions in the Upper Gastrointestinal Tract 🔬
Understand the causes, symptoms, and dangers of vomiting and upper gastrointestinal obstruction. Learn how early recognition, hydration, diagnosis, and fasting support gut rest — and when vomiting signals a medical emergency requiring immediate intervention.
GASTROINTESTINAL FASTING
Dr Hassan Al Warraqi
5/29/202511 min read


Vomiting and Obstructions in the Upper Gastrointestinal Tract 🔬
Understand the causes, symptoms, and dangers of vomiting and upper gastrointestinal obstruction. Learn how early recognition, hydration, diagnosis, and fasting support gut rest — and when vomiting signals a medical emergency requiring immediate intervention.
Understanding Upper GI Obstruction and Vomiting
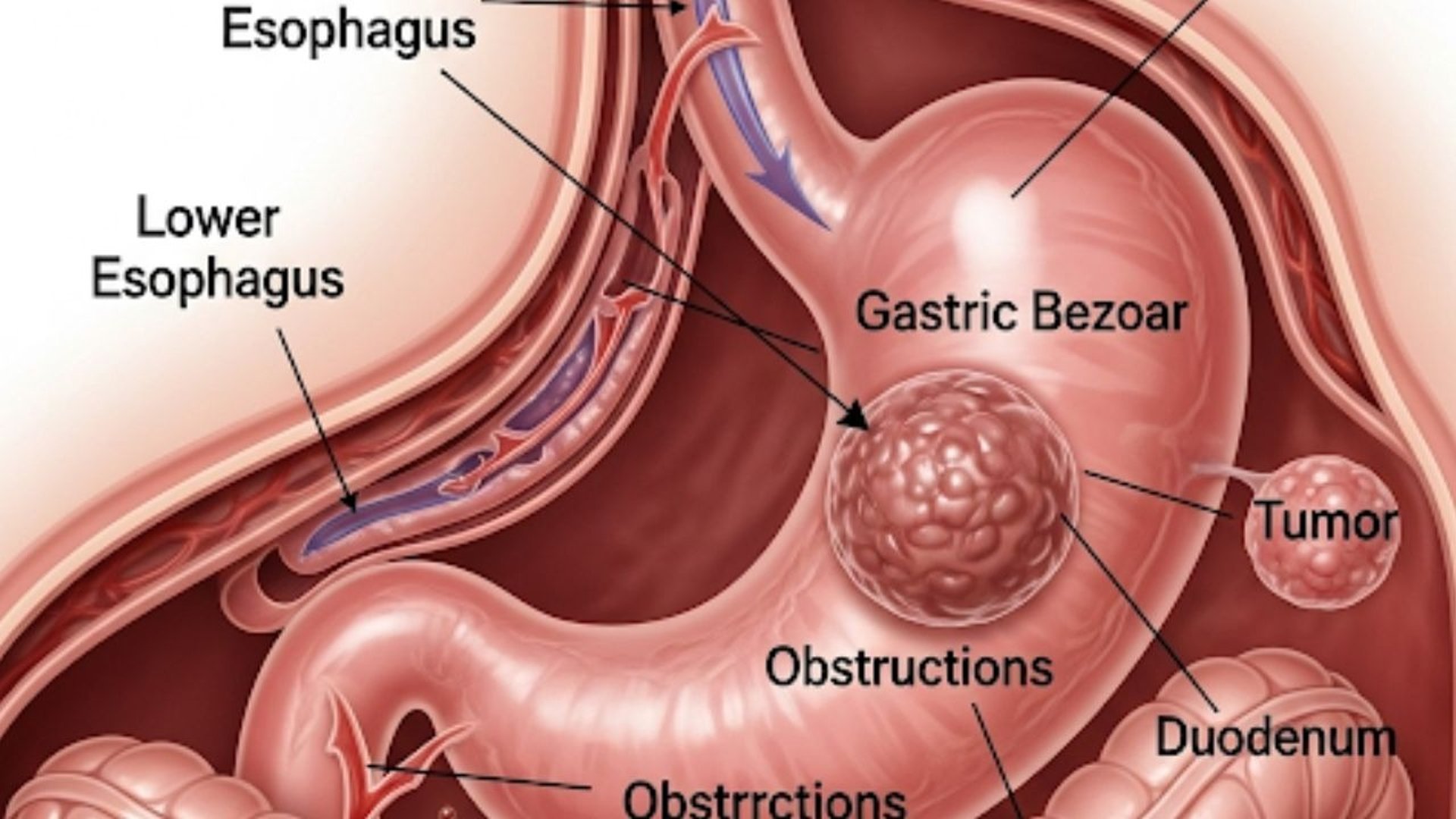
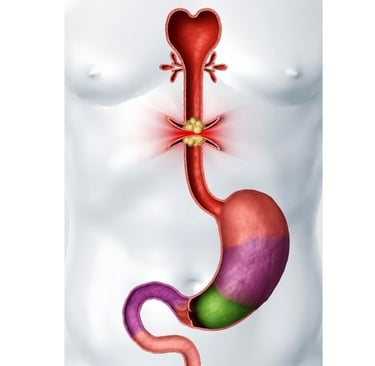
Upper gastrointestinal obstruction represents a serious medical condition where the normal passage of food, liquids, and digestive secretions becomes blocked anywhere from the esophagus to the proximal jejunum.
This blockage triggers a cascade of physiological responses, with vomiting being the most prominent and distressing symptom.
The pathophysiology involves mechanical impedance to gastric emptying, leading to progressive gastric distension.
As intragastric pressure rises, mechanoreceptors in the gastric wall activate vagal afferent pathways that communicate with the area postrema and nucleus tractus solitarius in the medulla oblongata.
This neural activation ultimately triggers the coordinated vomiting reflex through the central pattern generator in the medullary reticular formation.
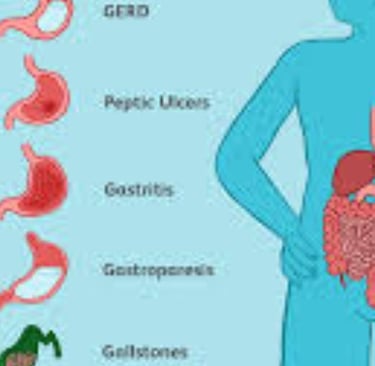
Detailed Classification of Upper GI Obstruction Causes
Esophageal Obstructions
Structural Abnormalities:
Esophageal strictures from gastroesophageal reflux disease (GERD) create progressive narrowing through chronic inflammation and fibrosis
Schatzki rings and webs represent focal areas of mucosal or submucosal narrowing
Congenital anomalies like esophageal atresia or tracheoesophageal fistula in pediatric populations
Neoplastic Causes:
Primary esophageal carcinomas, including squamous cell carcinoma and adenocarcinoma
Metastatic disease from lung, breast, or other primary sites
Benign tumors such as leiomyomas or gastrointestinal stromal tumors (GISTs)
Functional Disorders:
Achalasia involves failure of lower esophageal sphincter relaxation combined with absent esophageal peristalsis
Diffuse esophageal spasm creates uncoordinated contractions
Jackhammer esophagus characterized by hypercontractile peristalsis
External Compression:
Vascular rings and aberrant vessels compressing the esophagus
Mediastinal masses including lymphadenopathy or thyroid enlargement
Hiatal hernias with significant anatomical distortion
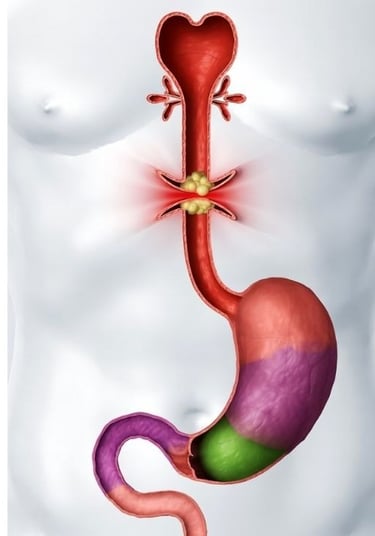
Gastric Outlet Obstruction
Peptic Ulcer Disease Complications:
Duodenal ulcers causing inflammatory edema and scarring at the pyloric channel
Gastric ulcers along the lesser curvature affecting gastric emptying
Chronic scarring from Helicobacter pylori-associated ulceration
Neoplastic Gastric Outlet Obstruction:
Gastric adenocarcinoma, particularly antral tumors
Pancreatic head carcinomas compressing the duodenum
Duodenal adenocarcinomas and periampullary tumors
Lymphomas affecting the gastroduodenal region
Congenital and Developmental:
Infantile hypertrophic pyloric stenosis with muscular hypertrophy
Congenital pyloric atresia or stenosis
Duodenal atresia and annular pancreas in neonates
Inflammatory Conditions:
Crohn's disease affecting the duodenum with stricture formation
Eosinophilic gastroenteropathy causing wall thickening
Caustic ingestion injuries leading to strictures
Duodenal and Proximal Jejunal Obstructions
Mechanical Obstructions:
Superior mesenteric artery syndrome compressing the duodenum
Gallstone ileus with impaction at the ileocecal valve
Bezoard formation from undigested material accumulation
Intussusception in pediatric populations
Inflammatory and Infectious:
Duodenal hematomas from trauma or anticoagulation
Parasitic infections like Ascaris lumbricoides causing bolus obstruction
Tuberculosis affecting the duodenum in endemic areas
Postoperative Complications:
Adhesive bands from previous abdominal surgeries
Anastomotic strictures following gastrojejunostomy
Afferent loop syndrome after Billroth II reconstruction
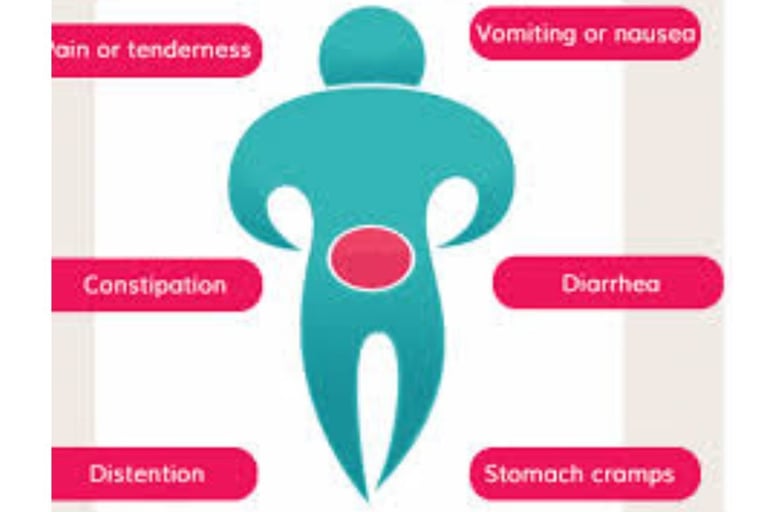
Clinical Manifestations and Symptom Patterns
Early Stage Symptoms
The initial presentation of upper GI obstruction typically involves subtle symptoms that progressively worsen. Patients experience postprandial fullness, early satiety, and intermittent nausea.
The vomiting pattern provides crucial diagnostic clues about the location and severity of obstruction.
Esophageal obstructions manifest as regurgitation of undigested food particles, often occurring within minutes of eating.
Patients may describe a sensation of food "sticking" in the chest, accompanied by substernal discomfort or pain. Unlike true vomiting, regurgitation lacks the forceful abdominal contractions and prodromal nausea.
Progressive Symptom Development
As obstruction becomes more complete, vomiting becomes more frequent and severe.
Gastric outlet obstruction produces characteristic vomiting of partially digested food that may occur several hours after eating.
The vomitus often contains recognizable food particles and may have a foul, fermented odor due to bacterial overgrowth in the stagnant gastric contents.
The timing relationship between eating and vomiting helps localize the obstruction level.
Immediate regurgitation suggests esophageal pathology, while delayed vomiting (4-6 hours post-meal) indicates gastric outlet or duodenal obstruction.
Advanced Complications
Chronic upper GI obstruction leads to significant nutritional consequences.
Progressive weight loss occurs due to reduced oral intake and malabsorption. Dehydration develops from persistent vomiting and reduced fluid intake.
Electrolyte imbalances, particularly hypokalemic hypochloremic metabolic alkalosis, result from loss of gastric acid and potassium.
Diagnostic Approach and Imaging Studies
Clinical Evaluation
The diagnostic workup begins with a comprehensive history focusing on symptom onset, progression, and associated factors. Physical examination may reveal gastric distension, visible peristalsis in thin patients, or a succession splash when shaking the patient's abdomen.
Laboratory Studies
Initial laboratory evaluation includes complete blood count, comprehensive metabolic panel, and liver function tests.
Electrolyte abnormalities commonly include hyponatremia, hypokalemia, and hypochloremia. Elevated blood urea nitrogen may indicate dehydration, while low albumin suggests malnutrition.
Imaging Modalities
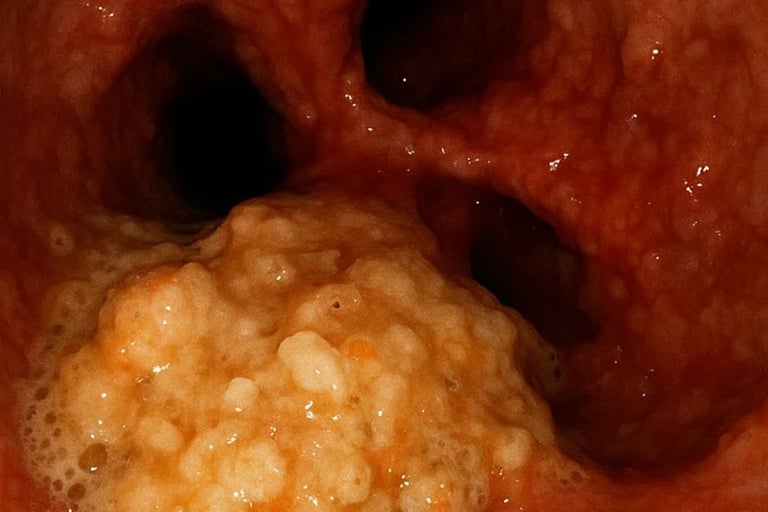
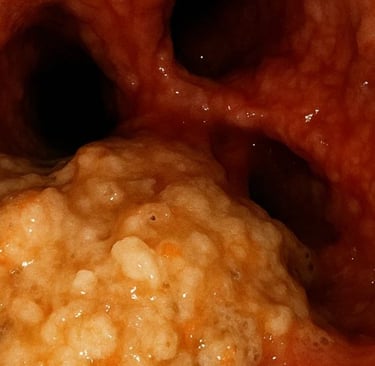
Upper Endoscopy: Provides direct visualization of mucosal abnormalities, allows tissue sampling, and enables therapeutic interventions like dilation or stent placement.
Upper GI Series: Barium studies outline anatomical abnormalities and demonstrate the level of obstruction through delayed gastric emptying.
CT Imaging: Cross-sectional imaging identifies masses, external compression, and complications like perforation or abscess formation.
Nuclear Medicine Gastric Emptying Studies: Quantify gastric emptying rates and help distinguish mechanical from functional obstruction.
Treatment Strategies and Management Approaches
Conservative Management
Initial treatment focuses on stabilizing the patient's condition through fluid resuscitation and electrolyte correction.
Nasogastric decompression relieves gastric distension and reduces vomiting episodes. Proton pump inhibitors reduce gastric acid secretion and may help with associated peptic ulcer disease.
Endoscopic Interventions
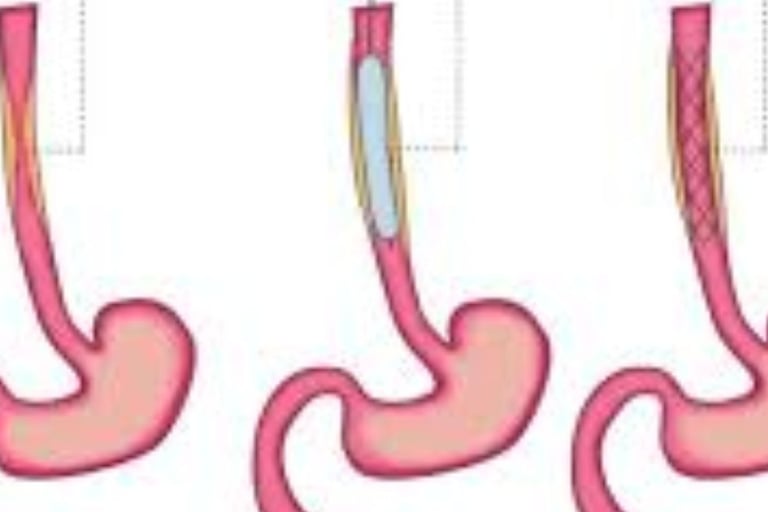
Therapeutic endoscopy offers minimally invasive treatment options for many obstructive conditions. Pneumatic dilation effectively treats achalasia and benign strictures.
Stent placement provides palliative relief for malignant obstructions. Endoscopic mucosal resection or submucosal dissection may remove small neoplastic lesions.
Surgical Management
Definitive surgical treatment depends on the underlying pathology and patient factors. Pyloroplasty or gastrojejunostomy bypass gastric outlet obstruction.
Esophagectomy may be necessary for malignant esophageal obstructions.
Laparoscopic approaches minimize surgical morbidity when technically feasible.
Complications and Long-term Outcomes
Immediate Complications
Aspiration pneumonia represents a serious risk from recurrent vomiting, particularly in elderly patients or those with altered mental status.
Mallory-Weiss tears can occur from forceful vomiting, potentially leading to upper GI bleeding.
Boerhaave syndrome, though rare, represents full-thickness esophageal rupture requiring emergency surgical intervention.
Chronic Consequences
Prolonged obstruction leads to gastric atony and delayed gastric emptying even after successful treatment. Nutritional deficiencies develop from malabsorption and reduced intake. Chronic dehydration may result in acute kidney injury, particularly in elderly patients with underlying renal disease.
Prevention and Risk Reduction
Primary Prevention
Early treatment of peptic ulcer disease and GERD reduces the risk of developing obstructive complications. Helicobacter pylori eradication prevents ulcer recurrence and associated scarring. Regular cancer screening in high-risk populations enables early detection of malignant causes.
Secondary Prevention
Patients with known risk factors require regular monitoring and surveillance. Endoscopic surveillance identifies early stricture formation or malignant transformation. Nutritional counseling helps maintain adequate intake despite anatomical limitations.
SEO-Optimized Content Summary
Upper gastrointestinal obstruction causing vomiting represents a complex medical condition requiring prompt recognition and appropriate treatment. Understanding the various causes, from peptic ulcer complications to malignant obstructions,
enables healthcare providers to develop effective treatment strategies. Early diagnosis through comprehensive evaluation and appropriate imaging studies improves patient outcomes and reduces complications.
The management approach must be individualized based on the underlying pathology, patient comorbidities, and severity of obstruction. While conservative measures may suffice for mild cases, severe obstructions often require endoscopic or surgical intervention.
Long-term follow-up ensures optimal outcomes and prevents recurrence.
🤢 Vomiting & Upper Gastrointestinal Obstruction: Complete Medical Guide
Vomiting is not a disease — it is a protective reflex. But when it becomes persistent, especially with pain or inability to eat, it can signal a serious upper GI obstruction.
Below is everything you need to understand it clearly.
🧬 1. How Vomiting Happens (Physiology)
Vomiting is controlled by a brain center called the Vomiting Center located in the medulla.
It is activated by:
🔹 1. Signals from the gut
Distension
Inflammation
Obstruction
Toxins or irritants
🔹 2. Chemicals in the blood
Uremia
Ketoacidosis
Drugs
Hormonal signals
🔹 3. Inner ear (motion sickness)
🔹 4. Higher brain centers
Emotions, severe pain, fear
Mechanism sequence:
Nausea
Salivation increases
Stomach relaxes
Diaphragm contracts violently
Abdominal muscles squeeze
Contents expelled
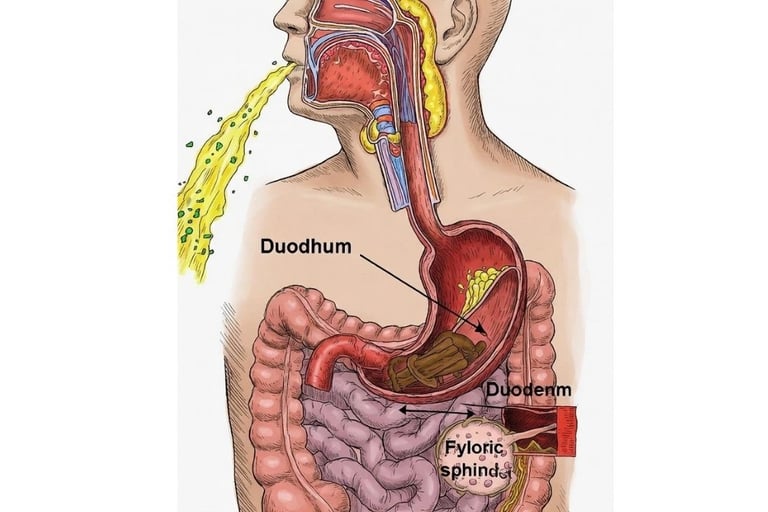
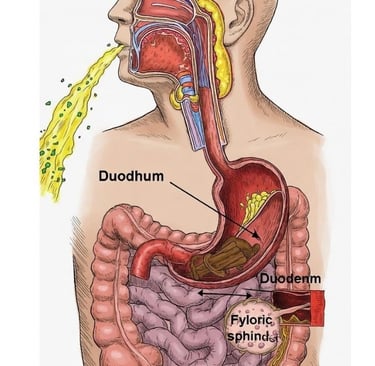
🚫 2. Upper GI Obstruction: What It Means
An obstruction means food and liquid cannot pass normally from:
Esophagus → Stomach
Stomach → Duodenum
This causes:
Severe nausea
Vomiting
Dehydration
Electrolyte imbalance
Abdominal distension
🔍 3. Causes of Upper GI Obstruction
A. Esophageal Obstruction
Strictures (acid reflux)
Tumors
Food impaction
Achalasia
External compression (thyroid, vessels)
Symptoms
Difficulty swallowing (dysphagia)
Food getting stuck
Regurgitation
Chest pain
B. Gastric Outlet Obstruction (GOO)
Blockage where the stomach empties into the duodenum.
Causes
Peptic ulcer scarring
Cancer of the stomach/pancreas
Pyloric stenosis (infants & adults)
Edema from severe gastritis
Foreign body ingestion
Symptoms
Projectile vomiting hours after eating
Vomit contains undigested food
Severe bloating
Dehydration
Visible gastric waves
C. Duodenal Obstruction
Congenital atresia
Pancreatic tumors
SMA syndrome
Adhesions
🚨 4. Red-Flag Symptoms (Seek Immediate Care)
Vomiting blood
Unable to keep liquids down
Severe abdominal pain
Green/Yellow bile vomiting
Rapid weight loss
High fever
Black stools
Persistent projectile vomiting
🧪 5. Diagnosis
Clinical Exam
Dehydration signs
Abdominal distension
Visible peristalsis
Succussion splash (sloshing sound)
Investigations
Endoscopy (most accurate)
Ultrasound
CT scan abdomen
X-ray (air-fluid levels)
Blood tests (electrolytes, kidney function)
💊 6. Treatment
A. Stabilization
IV fluids
Electrolytes
Antiemetics
Nasogastric decompression (NG tube)
B. Treating the Cause
Esophagus
Dilatation for strictures
Removal of foreign body
Botox or surgery for achalasia
Stomach / Duodenum
PPIs for ulcers
Endoscopic stent
Surgical correction
Tumor treatment
🌙 7. Role of Fasting in Vomiting & Upper GI Issues
🔹 1. Resting the Gut
Fasting gives the stomach time to:
Reduce inflammation
Decompress naturally
Decrease gastric acid output
Allow ulcers or gastritis to heal
🔹 2. Improves Motility
Short fasting cycles reset:
Gastric emptying speed
Duodenal movement
Vagal signals
🔹 3. Hormonal Stabilization
Fasting reduces:
Insulin spikes
Inflammatory cytokines
Gastric edema
Bloating
🔹 4. Helps Diagnose the Cause
If vomiting stops during fasting, the source is usually:
Food-triggered
Inflammation
Functional blockage
If vomiting continues even during fasting, the cause is more likely:
Mechanical obstruction
Tumor
Bezoar
This distinction is clinically important.
🍯 8. Role of Honey & Apitherapy (Supportive Only)
Not a treatment for true obstruction—but may help with:
Gastritis
Mild reflux
Mucosal healing
Reducing inflammation
But NOT for:
Tumors
Tight strictures
Foreign bodies
Pyloric stenosis
🧭 9. When Fasting is NOT Recommended
Severe dehydration
Persistent vomiting
Electrolyte imbalance
Obstruction confirmed by imaging
Vomiting blood
These require urgent hospital treatment.
🩺 10. Summary
Vomiting + upper GI obstruction is a serious condition that ranges from simple inflammation to life-threatening blockage.
Fasting helps functional causes, not mechanical ones.
Urgent medical evaluation is essential if symptoms are persistent, severe, or include red-flags.
Frequently Asked Questions (FAQs) about Emesis and Upper Digestive Tract Blockages
Q: What are the most common causes of upper GI obstruction leading to vomiting?
A: The most common causes include peptic ulcer disease with pyloric stenosis, gastric outlet obstruction from tumors, esophageal strictures from GERD, and duodenal obstructions. In infants, hypertrophic pyloric stenosis is the leading cause.
Q: How can I differentiate between mechanical obstruction and functional causes of vomiting?
A: Mechanical obstruction typically presents with consistent symptoms that worsen over time, visible gastric distension, and characteristic imaging findings. Functional causes often have intermittent symptoms, normal anatomy on imaging, and may respond to prokinetic medications.
Q: What are the warning signs that indicate urgent medical attention for GI obstruction?
A: Warning signs include severe dehydration, persistent inability to keep fluids down, severe abdominal pain, signs of perforation (fever, rigid abdomen), significant weight loss, or symptoms of aspiration pneumonia.
Q: How long does recovery take after treatment for upper GI obstruction?
A: Recovery time varies significantly based on the underlying cause and treatment method. Endoscopic interventions may provide immediate relief, while surgical procedures require weeks to months for full recovery. Chronic conditions may require ongoing management.
Q: Can upper GI obstruction recur after successful treatment?
A: Yes, recurrence is possible depending on the underlying cause. Benign strictures may re-stenose, requiring repeated interventions. Malignant causes have high recurrence rates. Regular follow-up is essential for early detection and management of recurrent obstruction.
Q: What dietary modifications are recommended for patients with upper GI obstruction?
A: Dietary recommendations include eating smaller, more frequent meals, thoroughly chewing food, avoiding hard-to-digest items, staying upright after eating, and maintaining adequate hydration. Liquid or pureed diets may be necessary for severe cases.
Q: Are there any medications that can help with symptoms of upper GI obstruction?
A: Prokinetic agents like metoclopramide may help with mild functional components, while proton pump inhibitors reduce acid secretion. Antiemetics can provide symptomatic relief, but definitive treatment usually requires addressing the underlying obstruction.
Q: What is the prognosis for patients with malignant upper GI obstruction?
A: Prognosis depends on the primary tumor type, stage, and patient factors. While curative resection may be possible for early-stage disease, advanced malignant obstruction often requires palliative interventions focused on symptom relief and quality of life improvement.
===================================================================================================================================================
🤢 Vomiting and Obstructions in the Upper Gastrointestinal Tract 🔬
Keywords
Treatment of gastric obstruction - Vomiting after eating - Symptoms of intestinal obstruction - Difference between mechanical and functional obstruction - When is vomiting serious?
✍️ About the Author
Hassan Al-Warraqi is the founder of H-K-E-M.com and a medical writer focused on digestive health, metabolic disorders, and natural interventions. With a deep interest in gastrointestinal physiology, Hassan breaks down complex topics like upper GI obstructions, vomiting mechanisms, and the systemic impacts of delayed gastric emptying.
His mission is to empower readers with evidence-based insights to recognize warning signs early and pursue informed, holistic care
.https://h-k-e-m.com/vomiting-and-obstructions-in-the-upper-gastrointestinal-tract-
Understand the causes, symptoms, and dangers of vomiting and upper gastrointestinal obstruction. Learn how early recognition, hydration, diagnosis, and fasting support gut rest — and when vomiting signals a medical emergency requiring immediate intervention.
=====================================================================================================================================================================================================
🩺 1. Understanding Long-Term COVID Vaccine Side Effects
Most people tolerate COVID vaccines well, but a small subset experiences prolonged or delayed side effects. These may include:
Fatigue and malaise
Muscle or joint aches
Brain fog / cognitive issues
Heart palpitations or mild myocarditis (rare)
Autoimmune-like reactions (rare)
⚠️ Most “long-term” side effects are mild and usually resolve spontaneously within weeks to months. Severe long-term effects are extremely rare.
These side effects are thought to be caused by:
Persistent low-grade inflammation
Immune system overactivation
Oxidative stress
Dysregulated autophagy (cellular cleaning process)
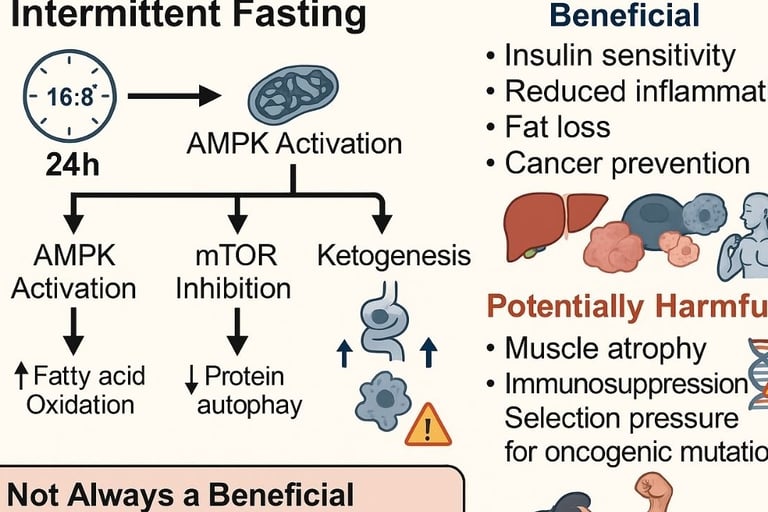
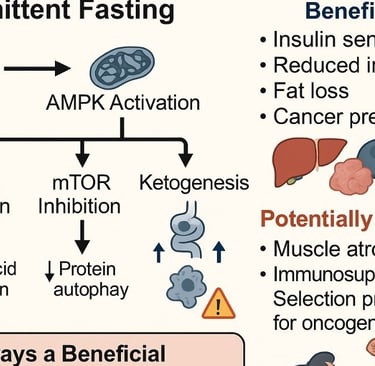
🧬 2. How Fasting Affects Your Body
Fasting—especially intermittent or periodic fasting—triggers a cascade of physiological responses:
Autophagy Activation
Fasting signals cells to recycle damaged proteins and organelles.
This may help clear spike-protein remnants or immune complexes linked to prolonged symptoms.
Reduction in Chronic Inflammation
Fasting reduces pro-inflammatory cytokines like IL-6 and TNF-alpha.
This may ease fatigue, muscle aches, and other inflammation-related symptoms.
Immune System Reset
Short-term fasting can promote immune regeneration and balance.
It encourages the production of new white blood cells, potentially modulating hyperactive immune responses.
Oxidative Stress Reduction
Fasting boosts antioxidant defense mechanisms.
Helps reduce cellular stress that can exacerbate symptoms like brain fog or muscle fatigue.
Metabolic Benefits
Fasting improves insulin sensitivity and mitochondrial efficiency, which can reduce fatigue and enhance energy metabolism.
⏳ 3. Types of Fasting That Might Help
3.1 Intermittent Fasting (IF)
Example: 16:8 (16 hours fasting, 8 hours eating window)
Benefits: Reduces inflammation, promotes autophagy, manageable long-term.
3.2 Periodic or Prolonged Fasting
Example: 24–48 hours water or very low-calorie fasting, once per month
Benefits: Strong autophagy induction, deeper immune reset
Caution: Must be supervised if you have chronic conditions or take medications.
3.3 Time-Restricted Eating
Example: Eating only within 6–10 hours daily
Benefits: Reduces oxidative stress and may stabilize circadian rhythm, supporting immune regulation.
🧠 4. Mechanisms Linking Fasting to Vaccine Side Effects
SymptomPotential Fasting MechanismFatigue / MalaiseEnhanced mitochondrial function, reduced inflammationMuscle achesReduced pro-inflammatory cytokines, improved cellular repairBrain fogIncreased neurotrophic factors, reduced oxidative stressAutoimmune-like reactionsReset of immune cell populations, improved regulationPalpitations / mild myocarditisAnti-inflammatory effects, better endothelial function
🔬 Animal studies and early human trials show fasting can modulate immune overactivation, which may indirectly alleviate prolonged vaccine side effects.
⚠️ 5. Safety Considerations
Hydration is essential — drink water, electrolyte beverages if fasting >24 hours.
Medical conditions — diabetics, heart conditions, or immune disorders should consult a physician.
Medication timing — some drugs require food; plan fasting carefully.
Start gradual — begin with 12–14 hour fasting before longer fasts.
✅ 6. Practical Recommendations
Start with 12–16 hour daily fasting for a few weeks and track symptoms.
Include anti-inflammatory foods during eating windows: leafy greens, berries, fatty fish.
Prioritize sleep and stress management — fasting amplifies benefits with proper rest.
Consider a supervised 24–36 hour fast once every 1–2 months if symptoms persist.
Monitor your body — if side effects worsen, stop fasting and consult a doctor.
🌟 7. Takeaways
Fasting may help reduce long-term COVID vaccine side effects by regulating immunity, reducing inflammation, and enhancing cellular repair.
Benefits are indirect and supportive, not a replacement for medical care.
Consistency, hydration, and safety are key.
Evidence is promising but still emerging; clinical trials specifically on COVID vaccine side effects are limited.
https://www.h-k-e-m.com/-can-fasting-help-with-long-term-covid-vaccine-side-effects
🩺 Can Fasting Help with Long-Term COVID Vaccine Side Effects?
==================================================================================================
====================================================================================================================================================================================================

















Get in touch
Address
Cairo Al Rehab
Contacts
+20 109 405 2056
hassanalwarraqi@h-k-e-m.com
