
Health is a crown on the heads of the healthy that only the sick can see.

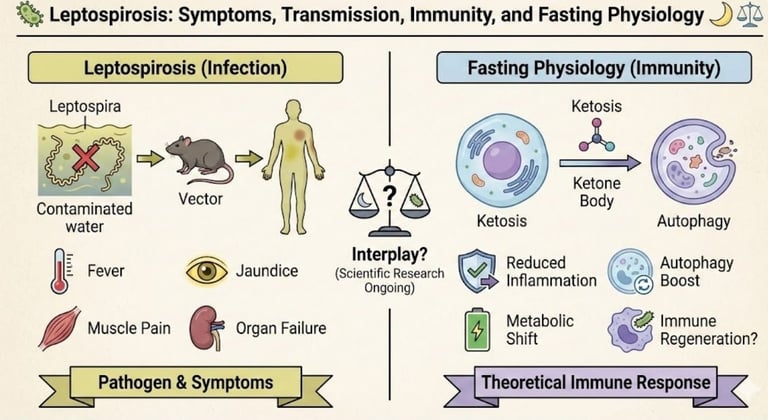
🦠 Leptospirosis: Symptoms, Transmission, Immunity, and Fasting Physiology 🌙⚖️
Complete medical guide to leptospirosis covering symptoms, transmission, immune response, diagnosis, treatment, and fasting safety during infection.
FASTINGKIDNY DISEASESAUTOIMMUNE DISEASESGENERAL
Dr Hassan Al Warraqi
1/3/202612 min read
🦠 Leptospirosis: Symptoms, Transmission, Immunity, and Fasting Physiology 🌙⚖️
/leptospirosis-symptoms-transmission-immunity-fasting
Complete medical guide to leptospirosis covering symptoms, transmission, immune response, diagnosis, treatment, and fasting safety during infection.
Leptospirosis is a significant global zoonotic disease caused by the Leptospira bacteria that poses a serious health risk wherever humans and infected animals interact.
While often associated with tropical climates and regions experiencing heavy rainfall, this infection can occur in any geographic location where contamination of water or soil has taken place.
Understanding the symptoms, transmission routes, risk factors, and the body's immune response is vital for effective prevention, early diagnosis, and successful recovery.
This comprehensive guide explores the clinical presentation, epidemiology, and emerging treatment approaches to leptospirosis.
What is Leptospirosis?
Understanding the Bacterium and Its Characteristics
Leptospirosis is caused by Leptospira interrogans, a highly motile, spiral-shaped bacterium characterized by distinctive hooked ends.
This unique morphology allows the bacteria to navigate through tissue and evade initial immune responses, making early detection and treatment critical.
The Challenge of Serova's and Strain Diversity
One of the most significant complications in managing leptospirosis is the existence of over 250 known servers (genetic variants or "strains") of Leptospira.
This remarkable diversity explains several clinical puzzles that healthcare providers encounter:
Diagnostic Complexity: The numerous servers make serological diagnosis challenging, as antibodies produced in response to one server may not cross-react with others, potentially leading to false negatives in standard testing protocols.
Variable Disease Severity: The clinical presentation varies dramatically between patients, from mild flu-like illness to life-threatening multi-organ failure.
Serova's differ in their virulence factors and tissue tropism, meaning different strains have different affinities for specific organs.
Geographic Distribution: Certain servers predominate in specific geographic regions, influenced by the local animal reservoir populations and environmental conditions.
Treatment Response: While antibiotics remain effective against all servers, the timing of administration and individual immune status significantly influence outcomes.
Zoonotic Nature and Reservoir Animals
Leptospirosis is fundamentally a zoonotic disease, meaning it naturally cycles between animal populations and occasionally spills over to infect humans.
Understanding the animal reservoirs is crucial for risk assessment and prevention strategies.
Rats are the most common source of human infection globally, but many other species maintain the bacteria in their kidneys and shed it through urine throughout their lives without showing clinical signs of illness.
How Leptospirosis Spreads
Transmission Routes and Risk Exposure
The primary and essential mechanism of leptospirosis transmission is direct contact with urine from infected animals or exposure to water and soil contaminated by that urine.
Leptospira bacteria can survive for weeks or even months in appropriately moist environmental conditions, creating a persistent risk in contaminated areas.
Common Routes of Infection and Exposure Scenarios
Contaminated Water and Soil Exposure
The majority of human leptospirosis cases occur through environmental contact.
The bacteria gains entry through splash contamination of the eyes, nose, or mouth, or through percutaneous penetration via cuts, abrasions, or breaks in the skin.
This is why wading in flood waters, swimming in potentially contaminated freshwater, or working in wet soil poses significant risk.
Animal Reservoir Contact
Direct contact with infected animals or their bodily fluids represents another significant exposure route.
Occupational workers who handle animals or animal products face elevated risk.
Infected dogs may shed bacteria through urine for weeks after infection, creating a household risk if contact with urine occurs.
Water-Based Recreation
Activities involving freshwater exposure—swimming, water sports, wading—present substantial risk, particularly in areas with known rodent populations or after flooding events when water contamination is widespread.
Occupational Risk Groups and High-Risk Professions
Certain occupational groups face disproportionately higher risk of leptospirosis exposure
Agricultural Workers: Farmers and livestock handlers encounter infected animals and contaminated environments regularly.
Cattle, pigs, and other livestock can harbor Leptospira and shed it through urine.
Veterinary Professionals: Veterinarians and veterinary technicians have direct contact with potentially infected animals and their biological materials.
Sewer and Sanitation Workers: Individuals working in sewage systems and contaminated water environments face routine exposure to rodent-infested areas.
Slaughterhouse and Meat Processing Staff: Occupational exposure to animal tissues and fluids places these workers at significant risk.
Wildlife and Environmental Workers: Those working with wildlife or in outdoor occupations in endemic areas face regular exposure.
Military and Emergency Personnel: Especially those deployed in tropical or developing regions with active leptospirosis circulation.
Symptoms and Clinical Disease Progression
Recognizing the Two Phases
Leptospirosis typically presents as a biphasic illness with distinct clinical phases, though not all patients progress beyond the initial phase.
Symptoms usually appear 5 to 14 days after exposure, though incubation periods can range from 2 to 30 days depending on bacterial load and route of exposure.
Phase 1
The Septicemic Phase (Acute/Mild Phase)
The initial phase mimics influenza and typically lasts approximately 3 to 7 days.
During this phase, the bacteria circulates in the bloodstream and can be cultured from body fluids.
Cardinal Symptoms of the Septicemic Phase
Sudden Onset High Fever and Chills
The illness typically begins abruptly with fever often reaching 39-40°C (102-104°F).
The sudden onset distinguishes leptospirosis from many other infections that develop more gradually.
Severe Headache: Often one of the most prominent complaints, the headache can be incapacitating and unresponsive to standard pain relievers.
Myalgia and Muscle Aches: Severe muscle pain is characteristic, with notable predilection for the calf muscles, lower back, and thighs.
This localized muscle pain pattern is considered a classic clinical sign of leptospirosis.
Conjunctival Suffusion: Red, irritated eyes without purulent discharge is a distinctive sign that helps differentiate leptospirosis from dengue and other febrile illnesses.
The whites of the eyes appear inflamed, but there is no eye drainage.
Gastrointestinal Symptoms: Nausea, vomiting, diarrhea, and abdominal pain occur frequently, contributing to volume depletion.
Additional Constitutional Symptoms: Patients often report fatigue, malaise, and general feeling of severe illness disproportionate to objective findings.
At this stage, most patients seek medical care, and with appropriate antibiotic therapy, recovery typically occurs within 7-10 days with minimal complications.
Phase 2
The Immune Phase (Severe/Weil's Disease)
If treatment is delayed or absent, or in the case of particularly virulent servers or immunocompromised individuals, some patients progress to a severe second phase 3 to 7 days after the initial symptoms begin to resolve.
This phase is characterized by IgM antibody production and paradoxical worsening despite bacterial clearance from the bloodstream.
This second phase is historically called Weil's Disease.
Hepatorenal Involvement and Multi-Organ Failure
Acute Liver Dysfunction
Hepatitis develops with marked elevation of liver enzymes.
Clinical jaundice (yellowing of the skin and sclera) becomes apparent, reflecting severe hepatic dysfunction.
Patients may develop encephalopathy as liver failure progresses.
Acute Kidney Injury
Progressive renal failure is the most common cause of death in severe leptospirosis.
The kidneys may show acute tubular necrosis, and patients develop oliguria or anuria.
Hyperkalemia, metabolic acidosis, and uremic toxicity develop rapidly.
Meningitis and Nervous System Involvement
Leptospiral meningitis
occurs in a subset of patients, presenting with meningeal signs, severe headache, and CSF pleocytosis with lymphocytic predominance.
Pulmonary Hemorrhage
Internal bleeding, particularly in the lungs, can occur and represent life-threatening complications.
Hemoptysis
(coughing up blood) may occur, and acute respiratory distress can develop.
Myocarditis
Cardiac involvement can cause arrhythmias and cardiogenic shock.
Metabolic Derangement
Hypoglycemia, hypokalemia, and severe electrolyte abnormalities occur due to multi-organ dysfunction.
The mortality rate in Weil's Disease ranges from 5-15% even with modern medical care, emphasizing the critical importance of early diagnosis and treatment in the first phase.
The Immunological Response
Fasting, Autophagy, and Bacterial Immunity
There is growing scientific interest in understanding how various physiological states affect the immune system's ability to handle intracellular bacterial infections like leptospirosis.
While this represents an emerging area of research, understanding these mechanisms is relevant for comprehensive integrative care approaches.
Autophagy
The Body's Cellular Housekeeping System
Autophagy is a fundamental cellular process in which cells digest and recycle their own components, including damaged organelles and invading pathogens.
This process is particularly relevant to intracellular bacterial infections.
How Fasting Triggers Autophagy
Nutrient restriction and fasting states activate autophagy through multiple pathways including mTOR inhibition and AMPK activation.
Short-term fasting (24-48 hours) has been shown in research to increase autophagic flux throughout the body.
Xenophagy
Targeted Pathogen Elimination
Xenophagy is a specialized form of autophagy where the body specifically targets and digests intracellular pathogens.
Since Leptospira can reside within kidney cells, liver cells, and other tissues during infection, theoretically enhanced xenophagic capacity could help clear persistent bacteria.
Potential Immunological Benefits
Enhanced autophagy may contribute to improved bacterial clearance and could theoretically reduce the inflammatory burden that contributes to multi-organ failure.
Inflammation Modulation and Cytokine Storms
One of the primary mechanisms of organ damage in severe leptospirosis is the "cytokine storm"—an excessive and uncontrolled immune response characterized by massive release of inflammatory mediators including TNF-alpha, IL-6, and IL-8.
This excessive inflammation paradoxically causes organ damage beyond what the bacteria itself causes.
Fasting-Induced Anti-inflammatory Effects
Short-term fasting has been documented to reduce circulating inflammatory markers and may dampen the excessive immune response.
By moderating inflammation, fasting could theoretically reduce organ damage during infection.
Metabolic Shift to Ketosis
The metabolic shift that occurs during fasting increases ketone body production.
Ketones have been shown in research to have anti-inflammatory properties through histone deacetylase inhibition and other mechanisms.
Critical Medical Caution
When Fasting Is Contraindicated
Important Warning
Fasting is absolutely not a cure or replacement for antibiotic therapy in active leptospirosis infection.
During active bacterial infection, several factors make fasting potentially dangerous
Dehydration Risk
Leptospirosis causes gastrointestinal fluid losses, and patients are at high risk for volume depletion.
Fasting further reduces fluid intake at precisely the time when maintaining renal perfusion is critical.
Electrolyte Imbalances
The combination of vomiting, diarrhea, and renal dysfunction creates severe electrolyte abnormalities.
Fasting can exacerbate these life-threatening
imbalances.
Accelerated Kidney Damage
The kidneys are particularly vulnerable in leptospirosis.
Reduced perfusion from dehydration associated with fasting could accelerate acute kidney injury and progression to renal failure.
Metabolic Derangement
Fasting in the setting of severe infection can lead to dangerous hypoglycemia and further metabolic complications.
Antibiotics Remain the Essential Standard
Leptospirosis is a bacterial infection that can become fatal within days if untreated.
Doxycycline or penicillin-based antibiotics are highly effective if started early and remain the only evidence-based treatment with proven mortality reduction.
Appropriate Role of Supportive Care
While fasting is contraindicated during active infection, supportive care measures including proper hydration, electrolyte management, nutritional support, and in severe cases dialysis and intensive care are essential.
Diagnosis, Treatment, and Prevention
A Comprehensive Approach
Diagnostic Methods and Challenges
Leptospirosis diagnosis is complicated by the similarity of early symptoms to other common febrile illnesses including dengue fever, malaria, influenza, and hepatitis.
PCR Testing
Polymerase chain reaction testing can detect Leptospira DNA in blood and urine during the first phase of illness.
This is the most sensitive test early in disease when bacterial load is high.
Results are available within 24-48 hours.
Microscopic Agglutination Test (MAT)
The gold standard serological test, MAT detects antibodies (particularly IgM) to specific servers.
However, antibodies don't appear until around day 5-7 of illness, limiting usefulness in early diagnosis.
MAT can determine which server is responsible, providing epidemiological information.
Culture
Leptospira can be cultured from blood during the first phase, but culture is slow (taking weeks) and not practical for clinical decision-making.
Rapid Diagnostic Tests
Point-of-care tests are increasingly available but have variable sensitivity and specificity.
Treatment Protocols and Clinical Management
Early Antibiotic Therapy
Prompt antibiotic therapy is the cornerstone of treatment and dramatically improves outcomes.
Doxycycline
100 mg twice daily for 7 days is the preferred agent for uncomplicated cases when started early (within the first week).
Doxycycline penetrates tissue well and achieves good concentrations in kidney and liver.
Penicillin
High-dose penicillin is used for severe cases and in patients who cannot tolerate doxycycline (such as pregnant women).
IV penicillin G is the standard in hospitalized severe cases.
Alternative Agents
For penicillin-allergic patients, ceftriaxone or chloramphenicol can be used, though these are less commonly used.
Hospitalization and Intensive Support
Severe cases require hospitalization for
Intravenous fluid resuscitation with careful monitoring to maintain renal perfusion while avoiding overload
Dialysis for acute kidney injury and renal failure
Respiratory support ranging from supplemental oxygen to mechanical ventilation
Vasopressor support for hypotension and shock
Transfusion support if hemorrhage occurs
Glucose and electrolyte management
Organ-Specific Management
Each organ system involved requires targeted management—ICU care for respiratory failure, nephrology consultation for renal failure,
hepatology involvement for liver failure.
Prevention Strategies and Risk Reduction
Avoiding Environmental Exposure:
Do not wade or swim in freshwater bodies, particularly after flooding or in areas with known rodent populations
Avoid contact with floodwater during heavy rains
Do not handle dead animals, particularly rodents
Use caution when working outdoors in damp conditions
Protective Equipment and Occupational Safety:
Wear rubber boots and waterproof gloves when working with potentially contaminated soil, water, or animals
Use proper personal protective equipment in occupational settings with exposure risk
Practice rigorous hand hygiene after potential exposure
Shower and change clothes after potential exposure
Rodent and Animal Control:
Minimize rodent infestations around homes and workplaces through sanitation and trapping
Store food securely to discourage rodent attraction
Seal entry points to buildings
Properly dispose of animal waste
Pet and Livestock Protection
Ensure dogs are vaccinated against leptospirosis—vaccines are available for common servers and are highly effective in preventing clinical disease
Vaccinate livestock (cattle, pigs) against endemic servers in your region
Prevent pets from drinking from potentially contaminated water sources
Seek prompt treatment if pets show signs of illness
Community-Level Prevention:
Water treatment and proper sanitation reduce environmental contamination
Proper disposal of animal carcasses and waste
Public education about exposure risks
Surveillance and control of animal reservoirs in endemic regions
Dr. Hassan Al-Warraqi's Therapeutic Fasting Approach
Core Philosophy:
Dr. Al-Warraqi, founder of H-K-E-M (Healing, Knowledge, Energy, Metabolism), positions fasting as a foundational pillar of integrative medicine.
His approach blends ancient healing wisdom with modern metabolic science, viewing fasting as a comprehensive therapeutic intervention that addresses physical, mental, and spiritual dimensions of wellness.
It is not a one-size-fits-all protocol but a personalized healing strategy.
its in general 3-4 days per week , David fast .
Key Features and Protocol Structure:
Individualized Duration and Intensity: There is no fixed schedule.
Protocols are tailored to the individual's metabolic status and health condition.
They can range from shorter fasts (12-24 hours) to extended therapeutic fasts (3-7 days or more), with a common practice being 3-4 fasted days per week.
Tri-Phase Integration
Fasting is not isolated. It is part of a three-phase protocol:
Pre-Fast (Preparation): A gentle dietary transition to prepare the body.
Fasting Period: Often includes supportive, mineral-rich broths or specific beverages to maintain electrolyte balance and support the body.
Post-Fast (Refeeding): A careful, strategic reintroduction of nutrient-dense foods to optimize healing and prevent adverse effects.
Focus on Chronic Disease Application:
The protocol is specifically designed to target and treat complex chronic conditions such as hypertension, diabetes, obesity, chronic kidney disease, and autoimmune disorders.
The goal is metabolic restoration, inflammation reduction, and cellular detoxification.
Emphasis on Metabolic Education
A crucial component is teaching patients to understand their own body's signals—recognizing adaptation phases, true hunger vs. dysregulated appetite, and signs of entering deep cellular healing states like ketosis and autophagy.
Safety and Medical Supervision
Given Dr. Al-Warraqi's background, his method heavily emphasizes safety.
This includes medical supervision for extended fasts, regular monitoring of metabolic markers, kidney function, and electrolyte balance, making it essential for individuals with health complications or on medications.
Suitability
This approach is particularly suited for:
Patients with complex, chronic diseases seeking a therapeutic intervention.
Individuals who require medical supervision and a highly personalized plan.
Those interested in a holistic protocol that integrates fasting with detoxification and nutritional strategies for comprehensive healing.
In essence, Dr. Al-Warraqi's method is a medically-guided, restorative journey tailored to an individual's specific health needs, making it a powerful tool for disease reversal and metabolic reset under professional care.
Frequently Asked Questions About Leptospirosis
Q: Can I treat leptospirosis with fasting instead of antibiotics?
A: No. Leptospirosis is an acute bacterial infection that can become fatal within days if untreated.
Antibiotics are essential to kill the bacteria and prevent progression to organ failure and death.
While fasting has theoretical immunological benefits in some contexts, it is dangerous in active leptospirosis infection due to dehydration and electrolyte risks.
Antibiotic therapy is non-negotiable treatment.
Q: Is there a human vaccine for leptospirosis?
A: While highly effective vaccines exist for dogs and some livestock, they target specific serovars and are not widely available or used for humans in most countries.
Human vaccination programs exist in some endemic areas (such as parts of Southeast Asia) but are not routine globally.
Prevention relies primarily on hygiene, proper sanitation, occupational safety measures, and avoiding exposure to contaminated environments.
Q: What is the survival rate with appropriate treatment?
A: With early antibiotic treatment initiated during the septicemic phase (first 7 days), the prognosis is excellent and mortality is less than 1%.
However, if the disease progresses to Weil's Disease (the severe second phase), mortality increases significantly to 5-15% despite modern medical care.
This dramatic difference underscores the critical importance of early recognition and treatment.
Q: Why does leptospirosis specifically cause calf pain?
A: Myalgia with notable predilection for the calf muscles is a classic clinical sign of leptospirosis, though the exact biological mechanism for this localization remains incompletely understood.
Theories include preferential muscle tissue invasion, specific inflammatory mediator effects on muscle, or particular susceptibility of calf muscle tissue to ischemic injury.
The calf pain is so characteristic that it's considered a diagnostic clue when present with fever and other leptospirosis features.
Q: Can chronic leptospirosis develop?
A: True chronic persistent leptospirosis is rare.
However, some patients report prolonged fatigue and myalgia lasting weeks to months after acute infection, sometimes termed "post-leptospirosis syndrome."
This is distinct from persistent infection and likely represents post-infectious inflammatory effects rather than active bacteria.
Conclusion: An Integrative Understanding of Leptospirosis
Leptospirosis represents a complex zoonotic infection at the intersection of infectious disease, environmental health, occupational medicine, and immune physiology.
While antibiotic therapy remains the essential and proven treatment, understanding the broader context—transmission ecology, immune mechanisms, and risk factors—enables comprehensive prevention and optimal patient management.
Emerging research into immune modulation, autophagy, and inflammatory responses offers intriguing possibilities for future adjunctive therapies, but these remain investigational and should never replace conventional antibiotic treatment in active infection.
For healthcare providers and patients alike, leptospirosis demands respect, prompt diagnosis, and evidence-based treatment as the path to optimal outcomes.
Summary
Symptoms Biphasic: fever, muscle pain → organ failure.
Transmission Contaminated water/soil + animal urine.
Immunity Weak/strain-specific; prevention > vaccines.
Fasting Relevance Avoid during infection; weakens defense against severe disease.
===============================================================================================================================================================================================================================================================================================================================================
Tetanus emergency care prioritizes hydration and nutrition over fasting claims, emphasizing lifesaving fluids, electrolytes, glucose, protein intake, wound management, antitoxin therapy, and ICU support while rejecting dangerous misinformation about fasting during acute infections;
#TetanusEmergency #StopFastingMyths #HydrationFirst #NutritionSavesLives #MedicalEmergency #AcuteInfection #CriticalCare #WoundCare #Antitoxin #ICUCare #PublicHealth #PatientSafety #EvidenceBasedMedicine #EmergencyMedicine #hkem
🚑 Tetanus Emergency : is Hydration & Nutrition Over Fasting Claims 🩹🍎
https://www.h-k-e-m.com/-tetanus-emergency-is-hydration-and-nutrition-over-fasting-claims-
===============================================================================================================================================================================================================================================================================================================================================



Get in touch
Address
Cairo Al Rehab
Contacts
+20 109 405 2056
hassanalwarraqi@h-k-e-m.com
