
Health is a crown on the heads of the healthy that only the sick can see.
🏥 Fatty Liver to Hepatoma: The Dangerous Progression You Must Know
Learn how fatty liver can silently progress to fibrosis, cirrhosis, varices, and liver cancer (hepatoma). Discover early warning signs, prevention strategies, and natural interventions to protect your liver. 🩺🍃
GASTRENESTAL
Dr Hassan Al Warraqi
11/6/2024

🏥 Fatty Liver to Hepatoma: The Dangerous Progression You Must Know
Learn how fatty liver can silently progress to fibrosis, cirrhosis, varices, and liver cancer (hepatoma). Discover early warning signs, prevention strategies, and natural interventions to protect your liver. 🩺🍃
the dangers of fatty liver disease, liver cirrhosis, esophageal varices, and liver cancer:
Beware the Inevitable Fate of Fatty Liver Disease
Fatty liver disease, liver cirrhosis, esophageal varices, and liver cancer - these are all serious conditions that can have devastating consequences if left unchecked.
While they may seem like separate issues, they are actually interconnected, forming a dangerous progression that every person should be aware of.
How it will happen
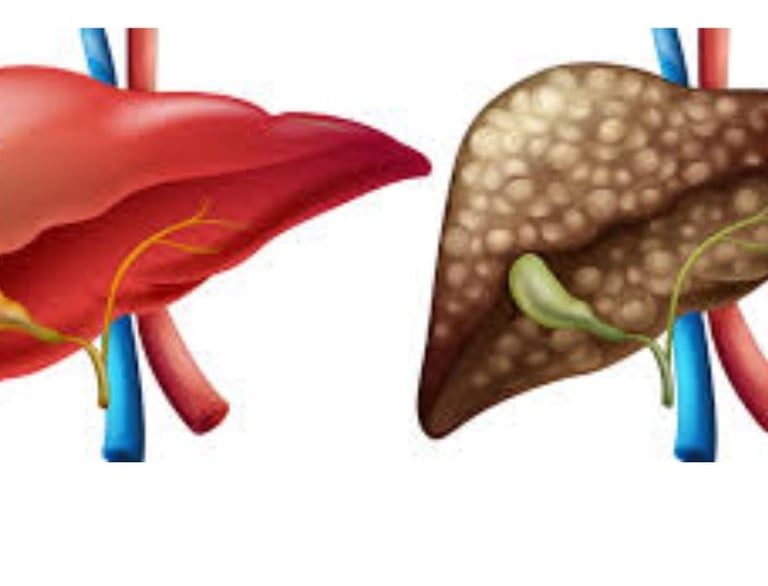
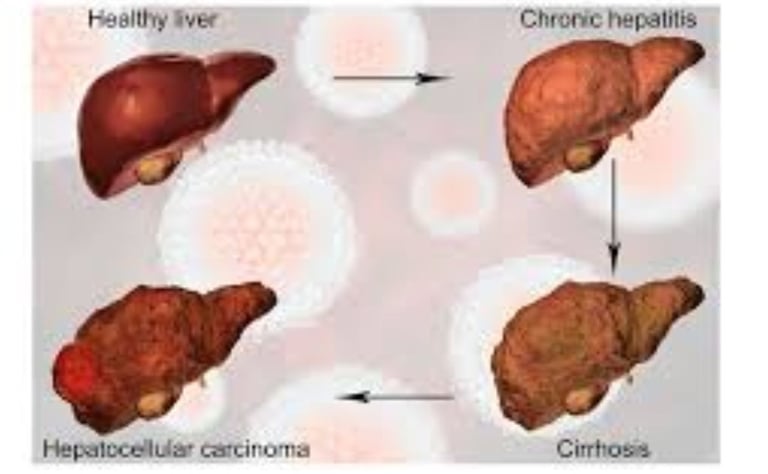
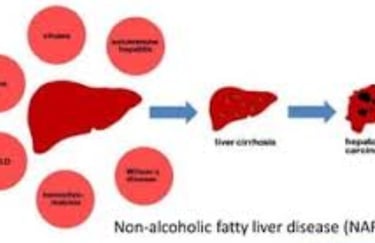
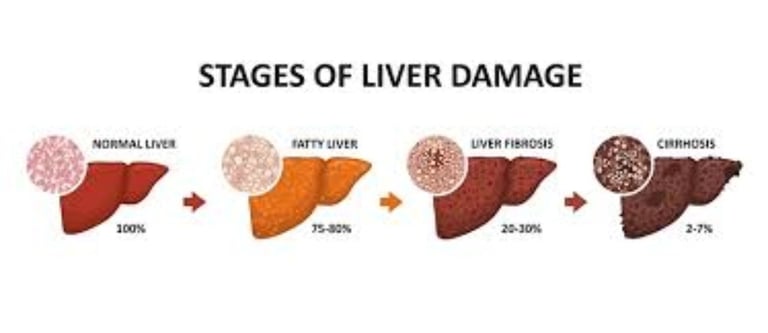
It all starts with fatty liver disease, a condition characterized by the buildup of fat in the liver.
This may sound relatively harmless, but make no mistake - fatty liver disease is the precursor to much more serious liver problems.
Causes
It is estimated that up to 25% of the global population has some degree of fatty liver disease, with the condition becoming increasingly common due to the rise of obesity, type 2 diabetes, and unhealthy lifestyles.
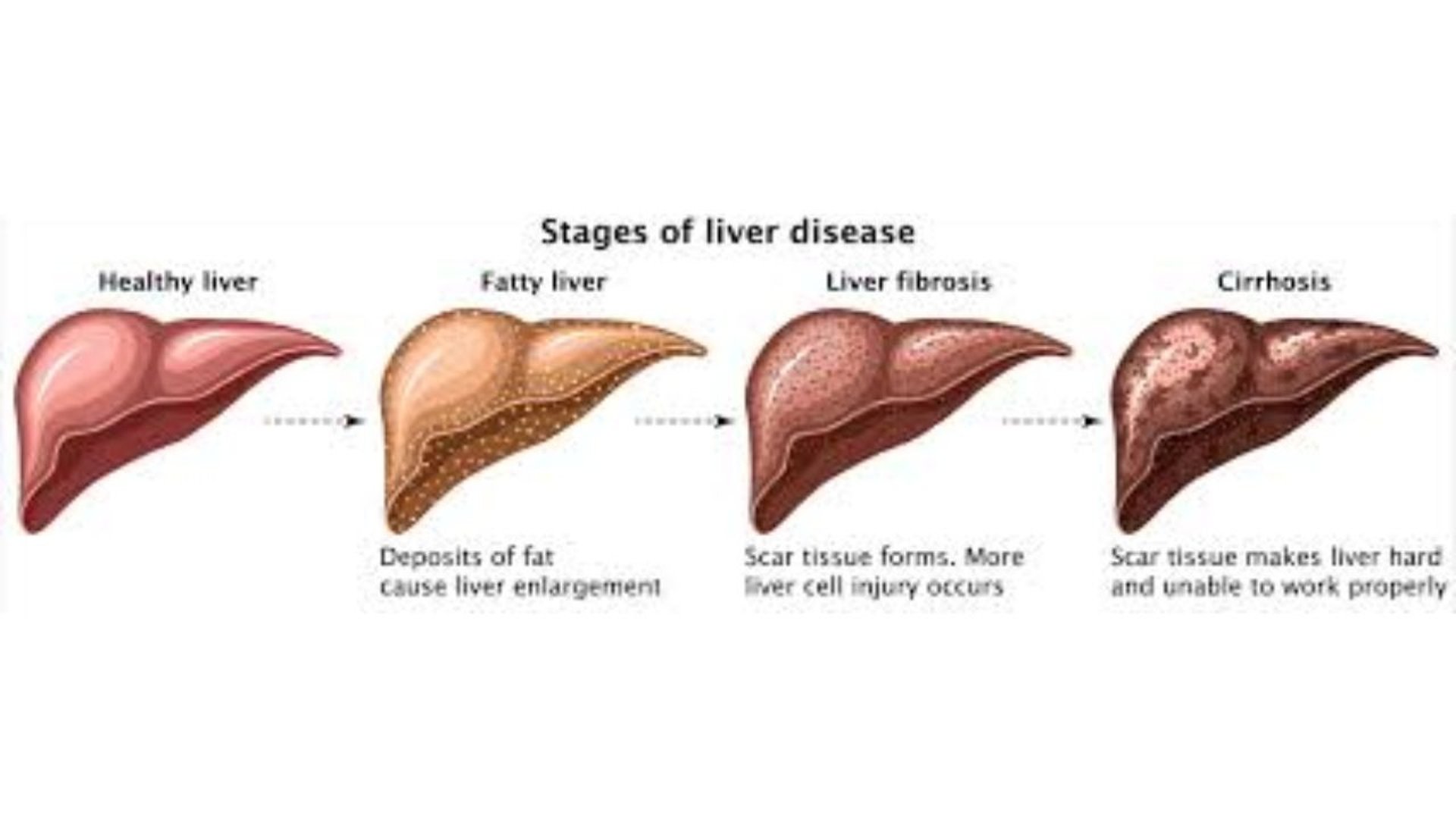
Stages
The initial stage of fatty liver disease, known as simple steatosis, typically doesn't cause any noticeable symptoms.
However, this benign-seeming buildup of fat sets the stage for the development of a more severe form of the disease known as nonalcoholic steatohepatitis (NASH).
NASH involves inflammation of the liver, which can lead to scarring and the formation of scar tissue, known as fibrosis.
Progression
As the fibrosis progresses, it can ultimately result in the development of liver cirrhosis - a advanced stage of liver disease characterized by extensive scarring and the loss of normal liver tissue.
Cirrhosis is a major risk factor for the development of potentially fatal complications, including esophageal varices and liver cancer. hepatoma ,
Esophageal varices
dilated veins that develop in the lower part of the esophagus as a result of increased blood pressure in the liver.
When these fragile veins rupture, they can cause life-threatening internal bleeding.
Individuals with cirrhosis have a 30-40% chance of developing esophageal varices, with the risk increasing the more severe the cirrhosis becomes.
And if the progression of liver disease wasn't already dire enough, cirrhosis also significantly increases the risk of developing liver cancer, specifically a form called hepatocellular carcinoma (HCC).
hepatocellular carcinoma (HCC) hepatoma
HCC is an aggressive cancer with a grim prognosis - the 5-year survival rate is only around 18%. Individuals with cirrhosis have a 2-8% annual risk of developing HCC, making routine screening and monitoring absolutely crucial.
The development of this cascade
of liver diseases does not happen overnight. It is a gradual, insidious process that can span years or even decades.
However, the consequences are severe, and the stakes are high. Fatty liver disease, if left unchecked, can inexorably progress to cirrhosis, esophageal varices, and ultimately, liver cancer.hepatocellular carcinoma (HCC)
Prevention
So what can be done to prevent this fate? The key lies in early detection and intervention. Unfortunately, fatty liver disease often goes undiagnosed in its early stages, as it typically causes no outward symptoms.
Regular check-ups and diagnostic testing, such as imaging scans or blood tests, are essential for identifying fatty liver disease before it has a chance to progress.
Further liver damage
Once fatty liver disease is detected, the focus shifts to managing the condition and preventing further liver damage.
This primarily involves addressing the underlying risk factors through lifestyle changes.
Losing weight, improving diet, and increasing physical activity can all help reduce liver fat and inflammation, potentially reversing the early stages of the disease.
For individuals with more advanced fatty liver disease or NASH, medications may also be prescribed to help control the condition.
Monitoring
Vigilant monitoring is also crucial, as it allows for the early detection of any progression to more severe stages of liver disease.
Regular check-ups, blood tests, and imaging scans can help identify the development of fibrosis, cirrhosis, or even the initial stages of liver cancer, enabling prompt intervention and treatment.
Cirrhosis
For those who have already progressed to cirrhosis, the stakes become even higher. Careful management of complications like esophageal varices and regular screening for liver cancer are essential.
Treatments may include medications, endoscopic procedures to address bleeding varices, and in some cases, liver transplantation - a complex and high-risk procedure that offers the best chance of long-term survival for individuals with end-stage liver disease.
The take-home message
is clear fatty liver disease is not a condition to be taken lightly.
It is the precursor to a cascade of increasingly severe and potentially life-threatening liver diseases.
By understanding the risks, seeking early diagnosis, and taking proactive steps to manage the condition, individuals can dramatically reduce their chances of facing the grim fate of cirrhosis, esophageal varices, and liver cancer.
Prevention is key
as the progression of liver disease is largely avoidable with timely intervention.
But for those who have already reached the advanced stages, diligent monitoring and aggressive treatment are essential for minimizing the risks and prolonging life.
Ultimately, the fight against fatty liver disease and its consequences requires a multi-pronged approach, involving both personal lifestyle changes and close collaboration with healthcare providers.
disease progression
The road ahead may be daunting, but with awareness, vigilance, and a commitment to proactive healthcare, the inevitability of this dire liver disease progression can be broken.
By taking action now, individuals can protect their liver health and safeguard their future well-being.
The choice is clear: take control of your liver health, or risk facing the devastating consequences of a preventable fate.
the alternative solution
role of dr hassan alwarraqi in the treatment by honey ,manuka honey and fasting outside ramadan
Honey and Manuka Honey:
Medical Applications:
Wound healing and burn treatment
Antibacterial properties, especially in Manuka honey
Treatment of diabetic foot ulcers
Sore throat and cough relief
Gastrointestinal health support
Unique Properties of Manuka Honey:
Higher methylglyoxal (MGO) content
Stronger antimicrobial properties
UMF (Unique Manuka Factor) rating system
Enhanced wound healing capabilities
Fasting Outside Ramadan (Medical/Therapeutic Fasting):
Types:
Intermittent fasting
Time-restricted feeding
Alternate-day fasting david fasting
Extended fasting protocols
fasting the white days 13-14-15 of each arabic month
fasting 2 days per week monday and thursday .
Potential Benefits:
Metabolic health improvement
Weight management
Cellular repair processes (autophagy)
Blood sugar regulation
Inflammation reduction
Cardiovascular health support
The keywords
interconnect fatty liver disease progression (steatosis, NASH, fibrosis, cirrhosis), complications (esophageal varices, hepatocellular carcinoma), while therapeutic approaches include natural remedies (honey, specifically Manuka honey's antimicrobial properties) and medical fasting protocols (intermittent, therapeutic, time-restricted , or islamic fasting ) with emphasis on evidence-based implementation, patient monitoring, and clinical safety guidelines.
FAQS
Frequently Asked Questions About Fatty Liver Disease and Its Potential Treatments
1. What is fatty liver disease, and what are its main types?
Fatty liver disease refers to the excessive accumulation of fat in liver cells.
The two main types are:
Non-alcoholic fatty liver disease (NAFLD): Caused by non-alcoholic factors such as obesity and diabetes.
Alcoholic fatty liver disease (AFLD): Resulting from excessive alcohol consumption.
If left untreated, fatty liver disease can progress to severe conditions like liver cirrhosis and liver cancer.
2. What are the main risk factors for fatty liver disease?
Key risk factors include:
Obesity
Type 2 diabetes
Insulin resistance
Metabolic syndrome
High cholesterol and triglyceride levels
Advancing age
Family history of liver diseases
Certain medications (e.g., methotrexate, tamoxifen, amiodarone)
Pregnancy
Polycystic ovary syndrome (PCOS)
Sleep apnea
Excessive alcohol consumption significantly increases the risk of alcoholic fatty liver disease (AFLD).
3. What symptoms might indicate the presence of fatty liver disease?
In its early stages, fatty liver disease is often asymptomatic. As the disease progresses, symptoms may include:
Fatigue
Discomfort in the upper right abdomen
Nausea
Loss of appetite
In advanced cases, severe symptoms may occur, such as:
Jaundice (yellowing of the skin and eyes)
Abdominal swelling (ascites)
Swelling in the legs and feet
Bleeding from the esophagus or stomach
Skin changes such as spider veins, itching, and discoloration may also be observed.
4. Can fatty liver disease lead to serious complications, and is it fatal?
Yes, untreated fatty liver disease can lead to severe complications like cirrhosis, a permanent scarring of the liver that may result in liver failure. It also increases the risk of liver cancer (hepatocellular carcinoma).
Mortality associated with fatty liver disease is significant, with estimates indicating a 44% increase in deaths related to NAFLD.
5. What treatment options are available for fatty liver disease?
Currently, there is no specific medication to reverse fat accumulation in the liver. Treatment focuses on lifestyle changes, including:
Adopting a balanced diet rich in vegetables, fruits, whole grains, lean proteins, and omega-3 fatty acids
Regular physical activity
Weight loss
6. Is Manuka honey or voluntary fasting beneficial for fatty liver?
Some studies suggest potential benefits of intermittent fasting and the use of Manuka honey. Honey, particularly Manuka honey, is valued for its antioxidant and anti-inflammatory properties. Consuming it in moderation (2-6 times weekly) may help protect liver cells and reduce toxin-related damage.
7. What role do fasting and honey play in managing fatty liver disease?
Intermittent fasting or alternate-day fasting has been shown to:
Reduce fat accumulation in the liver
Improve insulin sensitivity
Enhance autophagy, a process that detoxifies the liver and reduces excess fat
Manuka honey's antioxidant and anti-inflammatory properties may protect liver cells and mitigate the effects of certain toxins.
8. What medications and substances should be avoided in fatty liver disease?
Certain drugs may harm the liver and should be avoided, including:
Statins (cholesterol medications)
Methotrexate
Tamoxifen
Amiodarone
Niacin
Certain antibiotics (e.g., erythromycin)
Corticosteroids
Over-the-counter pain relievers like aspirin, ibuprofen, and acetaminophen
Consult a doctor before taking any medication if you have fatty liver disease.
9. How is fatty liver disease classified and assessed?
Fatty liver disease is classified into grades based on the percentage of fat in the liver:
Grade 1 (Mild): Fat constitutes 5-10% of the liver, manageable through diet and exercise.
Grade 2 (Moderate): Fat accounts for 10-25% of the liver.
Grade 3 (Severe): Significant fat and inflammation in and around the liver, often progressing to advanced stages like fibrosis, cirrhosis, or liver cancer.






Get in touch
Address
Cairo Al Rehab
Contacts
+20 109 405 2056
hassanalwarraqi@h-k-e-m.com
